Johann Granted $1.47 Million to Continue Cutting-Edge Lung Cancer Clinical Trials
| What will lung cancer diagnosis and treatment look like in the future? Look no further than the research happening today at UAMS.
“We’re coming into the long-promised ‘future’ of cancer treatment,” said physician-scientist Donald J. Johann Jr., M.D. “For the last 50 years, the holy grail of cancer research has been being able to detect the presence of cancer with a simple blood test, known as a liquid biopsy, and treat cancer patients on an individualized basis, which is precision medicine.”
In pursuit of his quest, Johann was awarded a $1.47 million grant from the Food and Drug Administration (FDA) to continue a clinical trial to determine if new approaches can be developed to monitor and screen for lung cancer with a blood test.
Johann is an associate professor in the departments of Biomedical Informatics and Internal Medicine in the College of Medicine at the University of Arkansas for Medical Sciences (UAMS).
“Recent advancements in genetic sequencing technology, computational science and the ability to manage massive amounts of data have made this type of research possible,” he said. “The vision is to combine the power of these approaches with clinical knowledge to improve outcomes. This is the future of cancer medicine, and it’s all doable.”
An innovative and important aspect of this approach is called bioinformatics, a new field in research that uses computational tools to assess medical and public health information, often on a large scale, looking for previously unrecognized patterns that can affect medical and public health science in a broad range of ways.
Lung cancer is the leading cause of cancer-related deaths in the United States and the world, and the incidence in Arkansas has been higher than the national average for the past 20 years.
Researchers believe precision medicine is key to changing these statistics. The current standard treatment for early stage lung cancer is surgical removal of the tumor, with the addition of chemotherapy/radiation when the cancer has spread to nearby lymph nodes. However, the cancer often returns after two to the three years and is deadly.
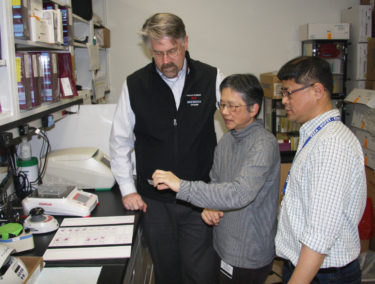
With Johann’s clinical trial, the surgeons are taking samples of the tumor at the time of its removal. Back in the lab, Johann’s team is running genetic sequencing on the tumor and re-growing it using different methods. Once the sample tumors are big enough, the team tests existing drugs and novel combinations of existing drugs on the tumors to find the most effective treatment.
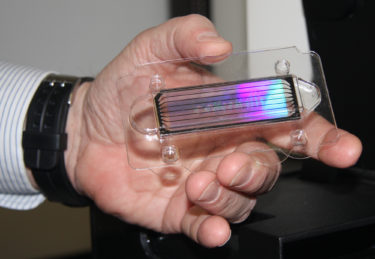
Johann shows DNA sequencing technology that is enabling his work. Today’s sequencing technology fits in the palm of your hand.
This information is analyzed and stored so that if that individual patient’s cancer comes back, their doctors will know the best medicines to use. The information is also compiled in large datasets so that researchers can look for aggregate patterns and identify trends regarding which treatments work best for different types of tumors. The idea is that now scientists will be able to genetically test a tumor to identify the best course of treatment for that individual patient.
Liquid biopsies are important because the average diagnosis for lung cancer patients is about age 70. Patients are often in poor health in addition to battling cancer, and traditional invasive biopsies can lead to complications or death.
Patients in Johann’s clinical trial are giving blood samples at multiple stages of treatment. The research team is determining whether the cellular material shed by tumors into blood can help doctors detect cancer earlier and monitor patients during cancer treatments to improve outcomes. Again, compiling big datasets plays a role.
The liquid biopsy part of Johann’s lung cancer work is also being supported by the Blood Profiling Atlas in Cancer (BloodPAC), a nonprofit consortium for data sharing between stakeholders in industry, academia and regulatory agencies with the goal of making liquid biopsies a reality.
BloodPAC is also supporting liquid biopsy clinical trials at Memorial Sloan Kettering Cancer Center for prostate cancer, University of Southern California for breast cancer, and University of Pennsylvania for pediatric cancers.
“The collaborative element to this is very important. We are working with three very prestigious, NCI-comprehensive cancer centers to accelerate the development of liquid biopsies for cancer treatment guidance and less invasive clinical care,” Johann said. “We want to catch disease early and operate on it for cure, be able to monitor it effectively, develop model systems effectively and then look at potential therapies to see what would be the best treatment for each patient, instead of just giving everyone the standard treatment.
“The practice of clinical oncology is rapidly changing, and we need to be part of that and contribute. When I came to UAMS, I believed we should be able to do state-of-the-art cancer research and treatment here. I’m proud to be part of this science, the teamwork and potential for our patients.”
Johann’s work on lung cancer has been underway for three years. During previous phases, his team developed the advanced bioinformatics and infrastructure at UAMS that are necessary to handle the large datasets involved in this research, and he brought firsthand knowledge of the latest molecular technologies to UAMS.
Johann completed fellowships in hematology oncology and clinical proteomics, both at the National Institutes of Health in Bethesda, Maryland. Johann earned his medical degree at Case Western Reserve University in Cleveland, Ohio. He became a physician as a second career, prior to attending medical school he was an engineering group leader for the Unisys Corp. and worked on advanced avionics projects.