Telemedicine Key to Physician’s Stroke Recovery
Telemedicine Key to Physician’s Stroke Recovery
| Robert Scott, M.D., on Dec. 9 lost almost all control he had over the right side of his body. He was having a stroke.
Less than three hours later, he had regained all its function with help from University of Arkansas for Medical Sciences (UAMS) neurologist Sami Harik, M.D., the AR Saves (Arkansas Stroke Assistance through Virtual Emergency Support) program and the staff at McGehee-Desha County Hospital.

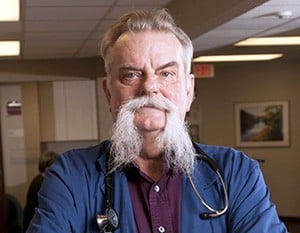
- Robert Scott, M.D, a physician in Dumas and Gould, credits SAVES and McGehee-Desha County Hospital staff with his quick recovery from a stroke.
On that Sunday morning in December, Scott had been preparing to do some cooking. He left his house to get a large skillet from a nearby storage building on his property. On his return, he was sweating and decided to remove his shirt but had trouble unbuttoning a cuff. Scott’s arm also gave him difficulty when trying to eat some yogurt, and that’s when he became convinced he was having a stroke.
Scott gathered up his medicine and told his wife what was happening. By that time, he could only give one-word answers to her questions. She drove him to the McGehee hospital. The nurses and physicians there quickly set up an AR SAVES video connection to UAMS so Harik could evaluate him from the Little Rock campus. Scott’s condition had deteriorated to the extent that he had no use of his right side.
Stroke patients are at high risk of death or permanent disability, but certain patients can be helped with the blood-clot dissolving agent tissue plasminogen activator (t-PA) if given within 4.5 hours of the stroke. The neurologist recommended t-PA for Scott, and the McGehee staff administered it to him through an intravenous drip.
“Once that was done, an hour later, I was back,” Scott said. “At this point, I have no known deficits.”
A former general surgeon, Scott now is a primary care physician and medical director working for the Daughters of Charity at St. Elizabeth Health Center in Gould and DePaul Health Center in Dumas.
He said the nurses and physicians at the McGehee hospital did just what they were supposed to do when he was brought in. SAVES added something extra, though, that was very needed.
“Having a neurologist who understands the intricacies, and monitoring what’s going on, and forming his own opinion is very valuable,” Scott said.
Ten years ago, he said, not much could be done for a stroke patient like himself except to put them on bed rest and monitor their condition.
“Now, if you get them quickly, you can do a lot,” Scott said. “A few years ago, the dice were in the air, and however it fell, that was how it was going to be.”
Driving two hours from his home to the UAMS campus would have eaten up precious time and that delay may have led to more lasting neurological damage from the stroke. SAVES brought neurological expertise there quickly and when it was needed.
Scott said he foresees nothing but growth for telemedicine, including more use with other specialists in non-emergency circumstances.
“Like all good ideas, it grows. As this develops, I anticipate we’ll have access to specialists as a regular thing, not just special circumstances,” Scott said. “I see this concept becoming more pivotal all the time, especially in rural environments. Not many doctors want to practice in a rural environment, which limits a patient’s access to health care without something like SAVES and telemedicine.”