View Larger Image

The patient in the immediate days after the scalp replantation
Medical Case Study – Scalp Reattachment
INITIAL CONTACT
A 21-year-old female patient with a traumatic total scalp avulsion was flown by helicopter from Russellville to UAMS.
She was working in a factory when machinery caught her hair and removed her scalp.
ASSESSMENT
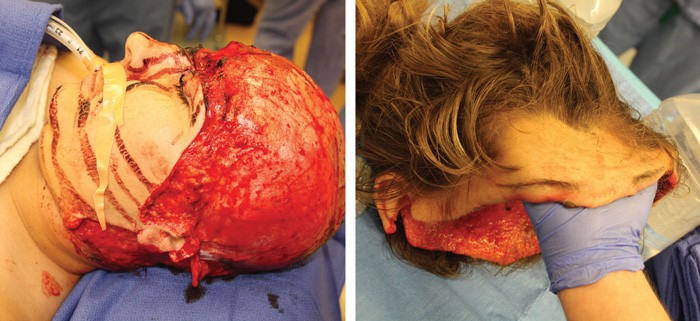
Left – Prepping the patient for surgery Right Completed arterial and venous microanastomosis The avulsed scalp
When head and neck surgeon Mauricio Moreno, M.D., met the patient, her wounds were covered in compressive bandages to prevent further bleeding. She was in shock, but awake and responsive.
Moreno discussed replantation with the patient and family. He explained that such cases are rare, with no guarantees of success. The more common procedure is to replace the scalp with skin graft from the abdomen or thigh.
The advantages of replantation include retaining her hair and the possibility to regain sensation and movement, as well as a better cosmetic outcome.
Challenges include the potential for blood loss, the complexity of the surgery and the potential for rejection or failure of the replantation.
The patient agreed to the replantation attempt and was in the operating room within three hours of the accident, which is within the acceptable timeframe for tissue replantation.
PROCEDURES
The surgery lasted from 7 p.m. to 5 a.m. Moreno was assisted by two otolaryngology chief residents.
The affected area of scalp extended from the nape of the neck, up and over to the forehead and included part of one eyelid. Both ears were affected, leaving only the lobes intact. Moreno has been able to find in recent medical literature fewer than 20 cases as complex as this one.
The patient was put under general anesthesia. The team performed a surgical debridement of her face to remove devitalized tissue. The first major task was to explore the temporal area and avulsed scalp to identify the stumps of the superficial temporal vessels. Excessive vascular damage would prevent the restoration of blood supply, making the replantation attempt moot.
Starting with the patient, they cleaned the vessels on both sides, trimming them back to healthy tissue. They moved to the scalp, cleaning and then trimming the hair and aggressively irrigating the tissue, followed by a debridement. They identified, cleaned and trimmed the transected vessels on both sides of the scalp.
The team proceeded to the next phase: microvascular anastomosis.
 The scalp was secured to the patient with a couple of holding stiches. The surgeons isolated the right-side artery on both the patient and the avulsed tissue and used a double Acland clamp to hold the two ends of the vessels together. Using 10-0 nylon suture in an interrupted fashion, they anastomosed the entire perimeter of the artery, which was approximately 2.5 mm in diameter.
The scalp was secured to the patient with a couple of holding stiches. The surgeons isolated the right-side artery on both the patient and the avulsed tissue and used a double Acland clamp to hold the two ends of the vessels together. Using 10-0 nylon suture in an interrupted fashion, they anastomosed the entire perimeter of the artery, which was approximately 2.5 mm in diameter.
Upon release of the clamps, a significant amount of blood flow returned to the scalp. It began to pink up and bleed around the edges, and blood began flowing out of the superficial temporal vein.
Working with the right-side vein, the technique was similar, except the surgeons used a venous coupling device to expedite the process.
Because of the rich vascular network of the scalp, it is possible to perform a replantation by anastomosing just one set of vessels. However, given the extension of the avulsed tissue, it was decided to proceed with a bilateral anastomosis.
The procedure was then repeated on the left side, bringing the total microsurgical time to about three hours.
The remainder of the surgery was devoted to a meticulous multi-layered reconnection of muscle, cartilage, lacerated nerves, skin, and scalp components. This painstaking process took about five additional hours, but restoring the anatomic continuity of all these structures was critical to achieve the best outcome.
Regarding the eyelid, Christopher T. Westfall, M.D., director of the Harvey & Bernice Jones Eye Institute, performed multiple subsequent surgeries to restore appearance and function.
FOLLOW-UPS
Moreno told the family the reattachment had been successful, but statistically there was a high chance for failure. It was now time to wait and see.

The patient in the immediate days after the scalp replantation
Moreno put the patient on a low dose of heparin as a prophylaxis for thrombosis. The patient was admitted to the progressive head-and-neck floor, a unit with a high nurse-to-patient ratio and where staff are specifically trained in flap care. Because UAMS performs a high volume of microvascular head-and-neck cases, the structure and staff were in place to care for the patient. Without this support, Moreno said he likely would not have attempted the surgery, because such care is so vital to successful outcomes.
In the days following, a small portion of tissue near the nape of her neck did not thrive. The blood flow to that area was outside of that provided by the reattached vessels.
She remained in the hospital for about a week. After a month, when the surgeons could be sure of the extent of the dead tissue, she returned to have it removed. The affected area was small enough – about 1.5 cm – that Moreno was able to simply join the edges of healthy tissue together. No skin grafting was needed.
The accident occurred in June 2014. By mid-2017, the patient had regained sensation in her forehead and was beginning to regain movement.
For consult or transfer, call 501-686-6080. To make a referral, call 501-526-1046.
Online Appointment Scheduling Faster, Easier, More Convenient Patient Appointment Registration
Now you can request appointments for your patients online. No more phone calls, transfers or waiting for a call back.
The Appointment Center will email you within 24-72 hours to assist with your appointment request. You will receive a faxed notification with the day and time once it is scheduled.
 Mauricio Moreno, M.D.
Mauricio Moreno, M.D.
Associate professor
Department of Otolaryngology – Head and Neck Surgery
UAMS College of Medicine
Education
Medical degree, Pontificia Universidad Católica de Chile School of Medicine
Residency
General surgery, University of Valparaíso, Chile
Otolaryngology – head and neck surgery, University of Chile, Santiago de Chile
Fellowship
Head and neck surgery visiting fellow, Department of Otolaryngology, University of Pittsburgh
Head and neck surgical oncology, Department of Head and Neck Surgery, the University of Texas, M. D. Anderson Cancer Center, Houston
Microvascular reconstructive surgery, Department of Plastic and Reconstructive Surgery, the University of Texas, M. D. Anderson Cancer Center, Houston
Surgical endocrinology, Departments of Surgical Oncology and Head and Neck Surgery, the University of Texas, M. D. Anderson Cancer Center, Houston
 Christopher T. Westfall, M.D
Christopher T. Westfall, M.D
Professor
Department of Ophthalmology
UAMS College of Medicine
Director
Harvey & Bernice Jones Eye Institute
Education
Medical degree, Ohio State University College of Medicine, Columbus
Residency
General surgery, Keesler U.S. Air Force Medical Center, Biloxi, Mississippi
Ophthalmology, Wilford Hall U.S. Air Force Medical Center, Lackland, Texas
Fellowship
Oculoplastic surgery, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston
