View Larger Image

John Lee singing and playing the ukulele.
Parkinson’s Patient Active and Proactive About His Condition Treatment
| May 14, 2018 | John Lee, of Little Rock, first noticed the small twitch in his fingers about seven years ago. He was in his 50s and Parkinson’s disease was at the top of his mind when he asked his primary care physician about it.
“My brother and my cousin both have it,” Lee said. “They’re younger than me.”
Lee’s uncle and grandfather were also diagnosed with Parkinson’s disease.
“With that kind of family history, you get a twitch and you start to wonder.”
At the initial visit to his doctor, Lee went through a series of cognitive and movement tests.
“He told me I was just a little nervous and prescribed me medication that would help me calm down,” Lee said.
The medication alleviated some of the symptoms, but Lee said it never really went away. He went back to his doctor two years later and this time his doctor referred Lee to Tuhin Virmani, M.D., Ph.D., co-director of the UAMS Movement Disorders Program. Virmani diagnosed Lee with Parkinson’s disease.
 Parkinson’s is a degenerative disease of the central nervous system that leads to a deficiency of dopamine, a chemical in the brain important for movement, but patients with Parkinson’s have a wide range of symptoms that include changes in mood, sleep patterns, constipation, urinary changes and even memory. Most patients, Virmani says, are diagnosed in their late 50s and 60s. Many factors that happen over a lifetime eventually lead to development of the disease. While there is a genetic component, primarily in young onset Parkinson’s disease, many are diagnosed with no family history.
Parkinson’s is a degenerative disease of the central nervous system that leads to a deficiency of dopamine, a chemical in the brain important for movement, but patients with Parkinson’s have a wide range of symptoms that include changes in mood, sleep patterns, constipation, urinary changes and even memory. Most patients, Virmani says, are diagnosed in their late 50s and 60s. Many factors that happen over a lifetime eventually lead to development of the disease. While there is a genetic component, primarily in young onset Parkinson’s disease, many are diagnosed with no family history.
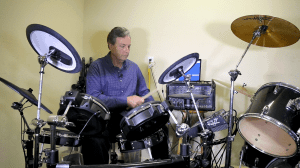
Since his diagnosis, Lee, a musician and broadcasting veteran, has been keeping busy voicing TV and radio commercials with Ron Sherman Productions in Little Rock. When he’s not working, he likes to make sure he’s active.
“I try to exercise as much as possible,” Lee said.
Exercise has been shown to potentially slow down the progression of Parkinson’s. So in addition to taking care of his six-acre property, Lee spends time playing drums (to keep his legs and arms busy) or singing and playing any of the variety of instruments he keeps in his music room.
The medication he takes, carbidopa/levodopa (or Sinemet), helps give the brain back the dopamine it is missing. Sinemet is the gold standard treatment for Parkinson’s patients, Virmani says, but it’s only one of the many treatments available for people in different stages of the disease. There is also deep brain stimulator surgery for people with more advanced disease. Lee visits Virmani every six months.
“He assesses my movements, asks me questions and has me memorize things,” Lee said. Then he laughs, “I’m terrible at memorizing. So I’m not sure what he can tell from that.”
He’s also a research participant in Virmani’s Gait Laboratory. Virmani studies a phenomenon in Parkinson’s disease where patients feel like their feet are “stuck or glued” to the ground, known as freezing of gait.
For the study, Virmani has patients walk on a mat so that he can objectively assess how their walking patterns change as the disease progresses.
“About 50-60 percent of patients with Parkinson’s develop freezing of gait,” Virmani said. “We’re trying to figure out why some do and others do not. Learning more about freezing of gait will help us develop therapies on how to slow its progression or prevent it from happening.”
Virmani says freezing of gait can cause a patient to lose his or her center of gravity, resulting in falls.
There is no cure for Parkinson’s disease, but Virmani stresses to his patients they can still live fulfilling lives decades after their diagnosis.
“They can still be functional members of society,” Virmani said. “And that’s our goal: to keep them as functional as possible for as long as possible.”