Neurostimulator Significantly Reduces Seizures for Missouri Man
| Matthew Pinegar was 3 months old when he had his first seizure. He was put on medication to keep them at bay, then taken off the medicine in junior high.
“It wasn’t until I was 21 when I had my first grand mal,” Pinegar said. “After that happened and I looked back, I’m sure I had lots of smaller seizures and just stopped noticing.”
A grand mal seizure is the most visible kind of seizure — a person loses consciousness and their body stiffens and jerks violently. But even smaller seizures can have a negative effect on the brain and a person’s health.
For Pinegar, having seizures was a part of his life, but they were a hindrance. Then came one grand mal that really changed his perspective. It happened Dec. 31, 2012. Carolyn Pinegar, his wife, was in the next room of their Nixa, Mo. home and thought he was hanging a picture on the wall.
“It sounded like a hammer at first,” she said. “Then something told me to go in there and check on him. I saw that he was having a seizure, his head banging repeatedly against the wall.”
Pinegar says after that episode, he experienced intense anger and had a hard time remembering everyday tasks. His neurologist eventually referred him to the UAMS Arkansas Epilepsy Center, the only epilepsy center in the state certified by the National Association of Epilepsy Centers.
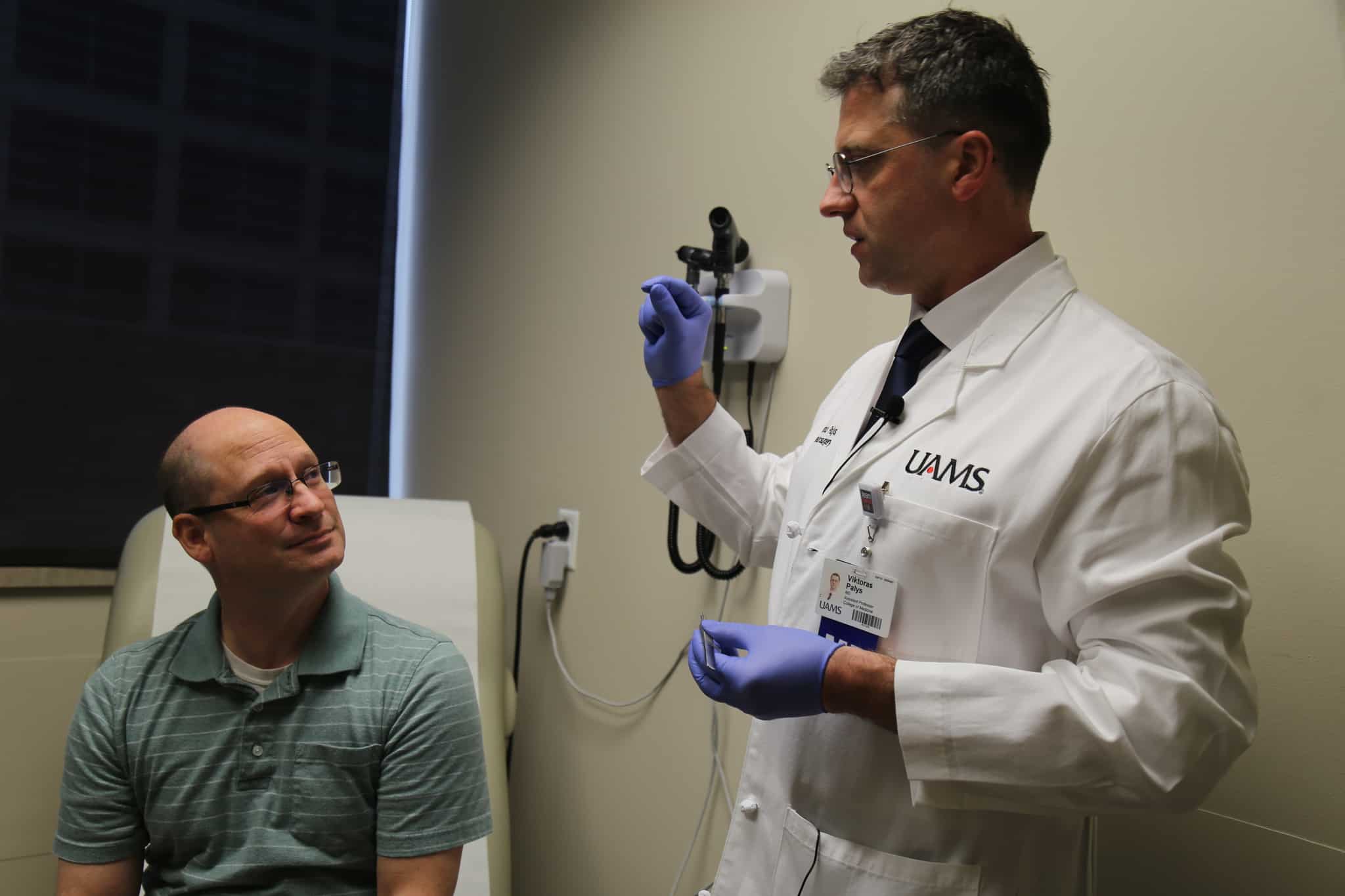
“Every time a person has a seizure, that part of the brain involved in the episode ages faster,” said neurosurgeon and epilepsy specialist Viktoras Palys, M.D., “You lose nerve cells because they get exhausted from generating electrical seizures discharges.”
Some patients have surgery to remove the part of the brain where the seizures start. But for patients like Pinegar – whose seizures originated in a part of the brain that cannot be removed – surgery was not an option, until recently.
Responsive neurostimulation (RNS) is the latest technology advancement in epilepsy surgery, best described as a pacemaker for the brain. RNS monitors electrical brain waves then responds when it senses a seizure. The system received FDA approval in 2013. Pinegar’s surgery was the first in Arkansas.
“In RNS surgery, you don’t have to remove the part of the brain that is causing seizures,” Palys said. “Instead you implant the RNS device with thin electrodes that go into the brain. It monitors the brain’s activity and responds when it senses a seizure.”
The neurostimulator, which is just over two inches long and an inch and a half across, is placed into the skull and the tiny wires put into the brain where the seizures originate. Pinegar’s surgery was Dec. 28 / 2018. He was able to go home the next day.
Weeks after the operation, his doctors could see the device had already intercepted nearly 50 would-be seizures. The device has memory storage and keeps track of the information. Nearly every day, Pinegar uses a device called a wand (It looks almost like a telephone receiver) to upload the neurostimulator’s data to a laptop.
“I just place the wand over the device and press this button on the laptop,” Pinegar said, demonstrating how it works.
In a matter of minutes, the wand communicates with the neurostimulator, uploading the information to an online database accessible by his neurologist. His doctors are able to review to see his brain activity, ensure the device is working properly and alternate treatment as necessary.
Most patients, Palys says, experience about a 70 percent seizure reduction after seven years. About 13 percent have become clinically seizure free, meaning the neurostimulator kept any seizures from causing symptoms.
It’s still too early after surgery for Pinegar to see all the benefits of RNS. But, so far, he’s happy with the progress in reducing seizures he’s already seen.