UAMS Researcher Pinpoints Immune System Cause for Autism Subtype
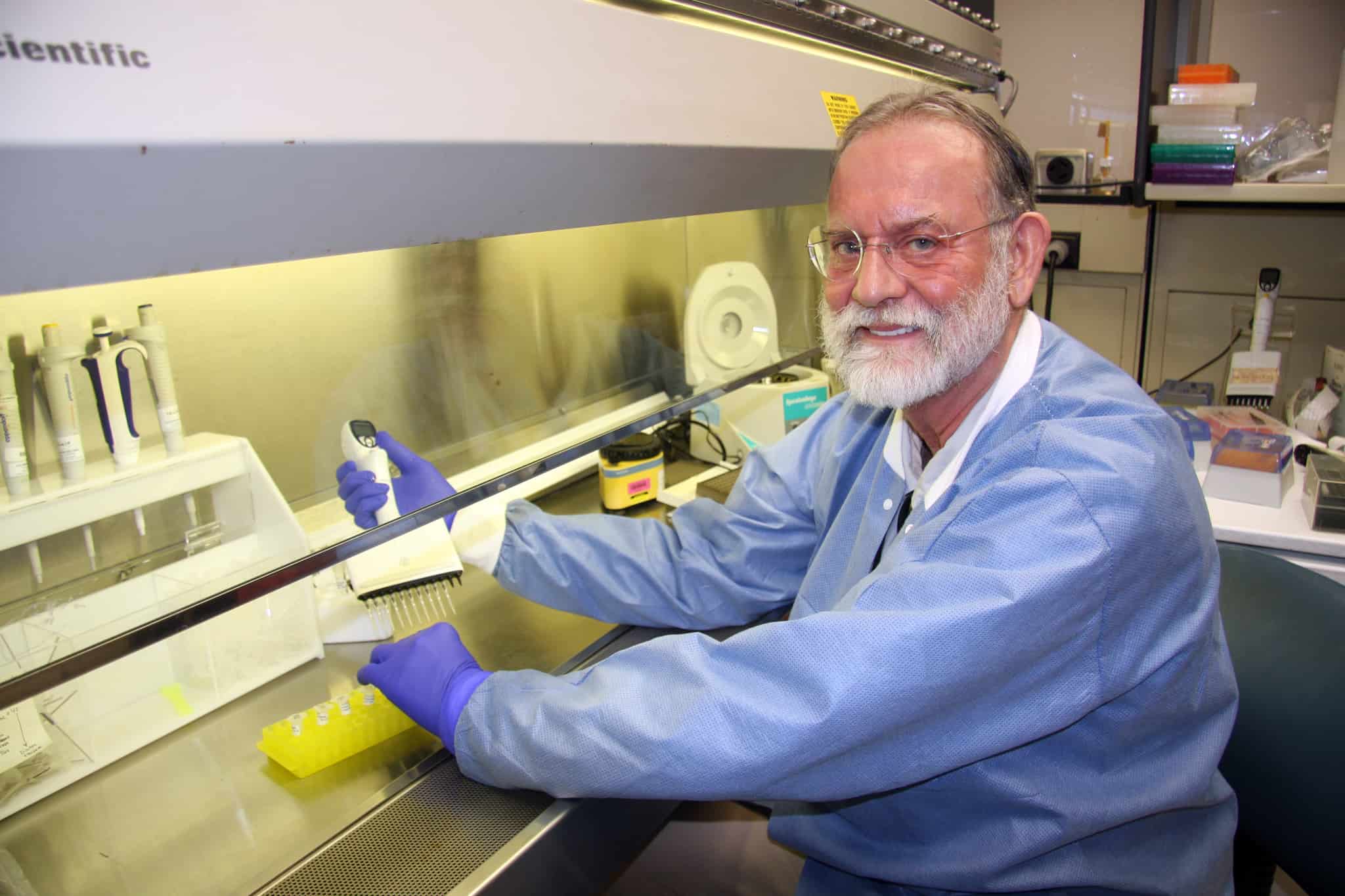
| Researcher Terry Harville, M.D., Ph.D., of the University of Arkansas for Medical Sciences (UAMS), has published a major study that for the first time links autism spectrum disorder to a specific genetic variation affecting the immune system.
The study, published in the Frontiers of Psychiatry, found that a genetically inherited immune type HLA-Cw7 was present in much higher numbers in people with autism as compared to the general population.
Harville and co-authors believe this HLA-Cw7 expression may cause chronic immune system activation for a subgroup of people with autism. In fact, this chronic inflammation may be affecting the brain and actually be causing the autism in these patients.
“Findings like this bring us one step closer to the future of treatment for autism: individualized medicine,” Harville said. “The more we truly understand the driving forces behind autism spectrum disorder, the better we will be able to identify and treat subgroups and individuals — to the maximum benefit for the individual patient.”
Harville, who is a professor of pathology and internal medicine at UAMS with a long career in pediatric immunology, collaborated on the study with the UAMS Department of Pediatrics, Arkansas Children’s Research Institute (ACRI), UAMS College of Public Health, National Center for Toxicological Research, and other institutions across the country.
Autism spectrum disorder includes a broad range of symptoms like challenges with social skills, repetitive behaviors, speech and nonverbal communication. It affects about 1 in 69 children in the United States.
While there is no known single cause of autism, the current consensus among the scientific community is that it is not one condition but several unique subtypes driven by both genetics and environmental factors. Scientists have long suspected the immune system may play a role for some subtypes, and a body of evidence is accumulating to support this connection.
Harville said it has been difficult to prove an immunological cause for autism, in part because the autism diagnosis is so broad. He agrees with the theory that autism is likely several different conditions, each with a unique cause. During his career as a pediatrician, Harville observed that the same treatment would have a dramatic effect for one patient with autism and little or no effect on another.
With this in mind, Harville’s study also attempted to identify other characteristics that define this subgroup of patients with the HLA-Cw7type. Harville found that — in addition to the behavioral symptoms that led to their autism diagnosis — these patients also reported higher rates of infections, allergies, food intolerances, chronic sinusitis and gastrointestinal issues compared to other patients with an autism diagnosis but without expression of the HLA-Cw7 gene.
“What emerges is a profile of symptoms that might help clinicians identify these patients as part of this subgroup,” Harville said. “Our next step will be looking at ways to perhaps manage these patients with treatments that alter immune system function or activation.”
Other variations of the HLA gene have been connected to autoimmune disorders like rheumatoid arthritis, celiac disease and ankylosing spondylitis. This led Harville to choose HLA for the focus of his autism study.
Individualized medicine, also called precision or personalized medicine, is the idea that advances in genetic testing, advanced computational abilities and other scientific tools are improving medical treatment by enabling it to be tailored to the individual.
UAMS co-authors on the study include Bobbie Rhodes-Clark, Ph.D., Department of Pathology; Sirish C. Bennuri, Marie Tippett, Shannon Rose, Ph.D., Stephen Kahler, M.D., Department of Pediatrics and ACRI; and Leanna Delhey, College of Public Health.
The study was funded by the Arkansas Biosciences Institute, the Jonty Foundation (St. Paul, Minnesota), the Autism Research Institute (San Diego), the Gupta Family Foundation (Atherton, California), the Jane Bostford Johnson Foundation (New York City), the Jager Family Foundation (Chicago) and the Phoenix Children’s Hospital Foundation (Phoenix). HLA typing was in part funded by research funds from the Department of Pathology in the UAMS College of Medicine.
UAMS is the state’s only health sciences university, with colleges of Medicine, Nursing, Pharmacy, Health Professions and Public Health; a graduate school; a hospital; a main campus in Little Rock; a Northwest Arkansas regional campus in Fayetteville; a statewide network of regional campuses; and eight institutes: the Winthrop P. Rockefeller Cancer Institute, Jackson T. Stephens Spine & Neurosciences Institute, Harvey & Bernice Jones Eye Institute, Psychiatric Research Institute, Donald W. Reynolds Institute on Aging, Translational Research Institute, Institute for Digital Health & Innovation and the Institute for Community Health Innovation. UAMS includes UAMS Health, a statewide health system that encompasses all of UAMS’ clinical enterprise. UAMS is the only adult Level 1 trauma center in the state. UAMS has 3,275 students, 890 medical residents and fellows, and five dental residents. It is the state’s largest public employer with more than 12,000 employees, including 1,200 physicians who provide care to patients at UAMS, its regional campuses, Arkansas Children’s, the VA Medical Center and Baptist Health. Visit www.uams.edu or uamshealth.com. Find us on Facebook, X (formerly Twitter), YouTube or Instagram.###