Schwartz Rounds Features UAMS’ First COVID-19 Patient
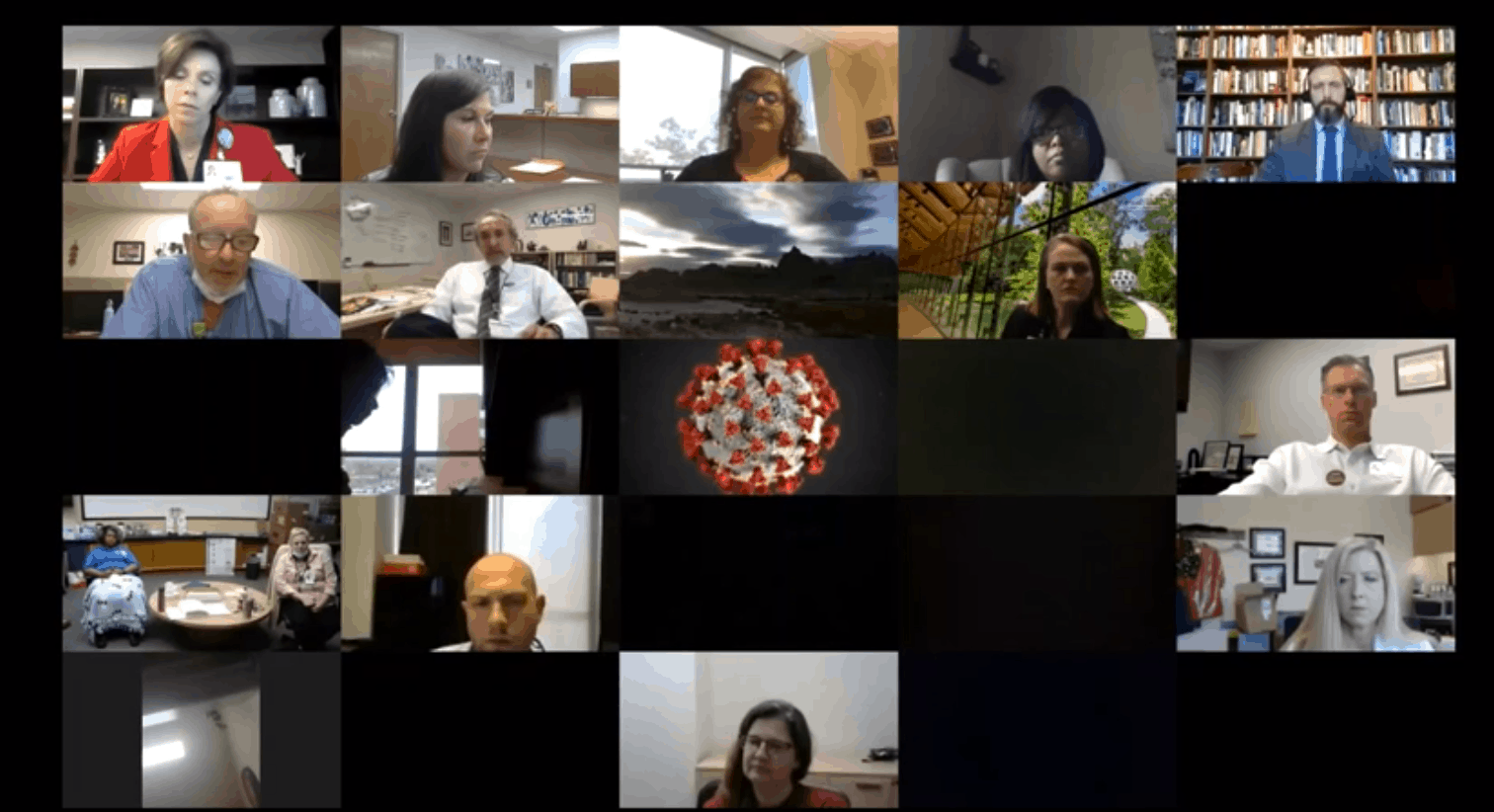
| On the one-year anniversary of Schwartz Rounds at UAMS, more than 180 employees and students participated in a virtual edition on June 17. The topic was “COVID Comes to UAMS: Caring for Our First Patient,” and the panel featured three health professionals who helped care for this patient.
Respiratory therapist Patrice Williams, R.R.T., Terry Brown, R.N., and Anand Venkata, M.D., shared their feelings about caring for the first COVID patient, who was admitted to UAMS on March 13. The patient was a male in his late 30s with no known exposure, and he had difficulty breathing when he came to the UAMS Emergency Department. He was discharged later that month after spending several days on a ventilator.
Brown talked about all the planning that went into patient placement and transfer in the weeks before the first patient arrived at UAMS, but he said very little discussion was focused on how staff would react to having to care for a COVID-positive patient. When the first one arrived, employees were hesitant to care for this patient because they were worried about their children, elderly parents or spouses with health conditions.
“I was very uncomfortable caring for him at first,” said Brown. “But with repetition, I got more comfortable and it got easier. He was very frightened, and he wasn’t able to get a deep breath. Every time I went in the room, he thanked me.”
Williams said she felt like she was on display during her first shift caring for the patient, with so many coworkers watching her and making sure she had all the personal protective equipment (PPE) she needed. She also talked about spending two hours with him, helping him talk to his family before he was intubated.
“The patient was terrified because of the unknown. Listening to him talk to his kids was a real tear-jerker for me,” said Williams. She also spoke of a second patient who looked at her with tears in his eyes and asked if he could hold her hand. His family couldn’t be there with him, so she held his hand throughout the intubation and worked with one hand.
“All I could do was hold his hand and say, ‘we’re here for you,’” she said.
Venkata said one of the first challenges was determining whether the patient had COVID. It took more than a day to get test results back, and during that time he ordered other tests to rule out other causes of his symptoms.
“Once the results came back, it was clear what we were dealing with,” he said. “The patient was very cooperative and helpful. He declined quickly, and his lungs were severely dependent on a breathing machine. We did the basics — we did them right — and he gradually improved. He spent four or five days in the ICU and had a good outcome.”
“I’m 100 percent more comfortable now than I was then,” said Williams. “We have more knowledge and more protection. It can be exhausting donning and doffing all the PPE, but actual patient care is just like any other patient.”
Respiratory therapist Tiffany Clarke, R.R.T., talked about how important the hospital staff was to her family when her father was hospitalized with COVID. He later died from the disease, and her message to panel was, “I appreciate you guys so much for doing that for the family, because I know how that family probably felt. Be patient. The phone is all they have. When they are calling, try to put yourself in that situation. Thank you and continue being compassionate.”
Following the session, UAMS Director of Pastoral Care Susan McDougal wrote to the panelists and Schwartz Rounds participants, “It is often in the hardest of times we find the best of ourselves and others. In the Schwartz Rounds yesterday we heard from colleagues who gave of the best of themselves in a time of uncertainty and suffering. Finding the blessing, feeling the warmth, the presence, in the care that was given helps us to carry on, to be proud of what we do, and of what has been accomplished. It also helps us forgive ourselves when we feel we are not at our best, knowing that we are human, and that our human-ness is what connects us and brings us closer together. To each one of you who spoke, and each one who wrote a thank you, and each one there who listened and cared, thank you for the blessing.”