Digital Health Visits Help Regional Campuses Meet COVID-19 Challenges
| Brittnay Hall, 39, was at an impasse: COVID-19 worries were making worse her pre-existing problems with anxiety. Also, thinking of having an in-person visit with her physician about her anxiety medications made her feel unsafe.
Digital health technology resolved her dilemma.
Hall, of Newark, had a more-than-20-year patient-physician relationship with Julia Roulier, M.D., a family medicine physician at UAMS Family Medical Center in Batesville.
A paralegal with a Batesville firm, Hall had been working from home to avoid potential exposure to COVID-19 in her workplace. That isolation was increasing her anxiety to the point where it was making it harder for her to focus on her work and fearful of a panic attack, although Hall was still able to function.
She wanted to talk to Roulier about that and to see if an adjustment in her medication would help, but she also was worried about possible exposure to COVID-19 patients in the Family Medical Center, which is a part of the UAMS North Central Regional Campus in Batesville.
“The Medical Center and Dr. Roulier accommodated me so that I could keep the appointment but do it over the live video connection,” Hall said. “That way I could see her and she could see me. I actually enjoyed it. It was extremely convenient, and I did get a lot of reassurance out of it.”
Roulier approved a change in her medication, and Hall felt better able to focus.
Hall wasn’t alone as a patient either. From mid-March through May, most patients visits with physicians and residents were seen through live video connections made possible by the UAMS Institute for Digital Health & Innovation. Curtis Lowery, M.D., is the director of the institute, which was established by UAMS in 2018.
Using the same software as UAMS HealthNow, the university’s online convenient care service, the institute facilitated the start and continuation of digital health patient visits at all eight of the UAMS regional campuses statewide.
Batesville accounted for about 40% of the remote patient visit volume at all the regional campuses.
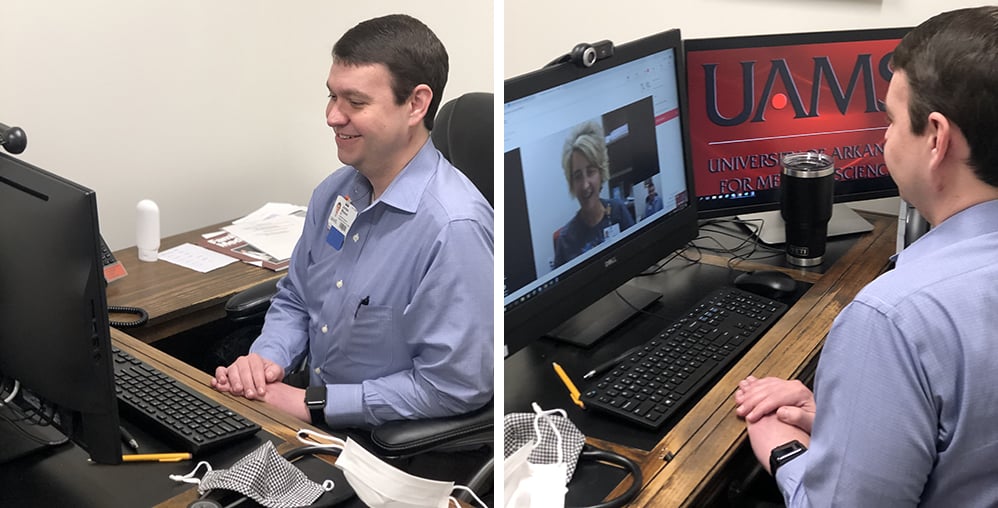
“We were the early adopters and guinea pigs for figuring out the work flows,” said Jordan Weaver, M.D., program director at the regional campus there. “We were a couple of weeks ahead of everybody and made a push for digital health. I was really pleased with it, and it’s easy to do if you know the patients and have already seen them in the clinic.”
Digital health is especially suited for consultations to go over results from medical tests or medication refills that are relatively routine, Weaver said. He and Family Medical Center physicians and staff tried to do as many over video as possible. It saved travel time for patients and even in some cases enabled patients to visit with a physician or advanced practice registered nurse from their workplace.
“The digital health live video was able to connect us to patients who were feeling isolated,” Weaver said. “In terms of educating patients about COVID-19, it also gave us opportunities to discuss social distancing and the proper use of masks if they do need to leave the home.”
Sometimes leaving home meant driving to the parking lot outside the Batesville clinic. Because of problems connecting to the internet in rural areas where some patients live, they drove to the parking lot and for the digital visit were loaned an iPad to connect and see their physician on the tablet, using the Family Medical Center’s wi-fi.
“I think you can obtain so much more information over live, digital health video compared to the phone. Some of the patients seem more comfortable and forthcoming in their conversations over interactive video, even more than in person or over the phone,” said Russell Mayo, M.D., Regional Campuses medical director.
Working with and leading the Institute for Digital Health & Innovation team tasked with bringing digital health patient visits to UAMS Regional Campuses were Marcia Byers, Ph.D., RN, director of clinical innovation and research for UAMS Regional Campuses; Terri Imus, B.S.N., RN, clinical director of the institute’s Go Live Team; and Teague Johnson, director of technology for the institute. The regional and institute teams had only three weeks to bring the first few campuses online.
“If we were trying to explain how to do this in another system, we would tell them it takes a number of people with strong skill sets in different specialties to be successful here,” Byers said. “You have to have clinical people, you have to have technology people and you have to have communications between them. I think that’s what Terri Imus and I are good at because we are both nurses and know both sides of it. You can’t be successful without all of those at the table.”
Byers said getting the technology in place that quickly was the first thing to do, but the even bigger challenge was making sure 250-350 nurses and staff at the different regional campuses were trained and ready to use the technology. That included integrating digital health patient care into billing and insurance processes and using it in coordination with electronic medical records.
She called Weaver “a champion” in thinking all that through for operations in Batesville and that was important in implementing digital health at the other seven regional campuses.
“Technology is one thing,” Johnson said. “Understanding work flows and the ability to comprehend an end-to-end pathway in which a patient or clinician starts in one place, goes through here and ultimately gets to an end. Once you can see that like Dr. Weaver did, you can adapt the technology to how you need to use it.”
Weaver said when in-person visits to the Family Medical Center started in May, digital health visits eventually decreased to roughly a quarter of the total patient visits. Nevertheless, patients and physician will continue to enjoy having the option of using the new technology, and Weaver sees it playing an increasingly central role as part of chronic disease management for conditions like diabetes or high blood pressure.
It will continue to be about caring about patients in the safest way that is best for them, and one of the patients who is sold on the idea is Brittnay Hall.
“It was such a smooth experience that I would do it again, even after the pandemic is over,” she said.