Little Rock Firefighter Survives COVID-19, Donates Plasma
| It was still early days in the sweep of COVID-19 across the country when John Fulbright of Cabot, a paramedic and firefighter in Little Rock, found himself admitted to UAMS with shortness of breath and fever.
“After I was hospitalized, it got worse before it got better. I was little concerned about being put on a ventilator, because that’s all you were hearing about on the news at the time – the worst case scenarios,” he said. “I thought about the last time I’d hugged my wife and wondered if that really would be the last time or if I’d ever see my kids again.”
It had all happened so quickly. A headache and chills (“which was odd for me, I’m always the warm one in the house”) on Sunday turned into a fever on Monday. Fulbright had heard enough to call the state Department of Health, which sent him to a drive-thru testing at UAMS Medical Center.
Three days later, Fulbright learned he’d tested positive. The day after the results came, Fulbright’s shortness of breath made speaking difficult, and he was advised to contact the UAMS Emergency Department, which coordinated his safe admission to the hospital. Meanwhile, his wife also tested positive for COVID, though her symptoms were not as severe and would only last three days.
“The doctors came in on my first day in the hospital and put me at ease,” Fulbright said. “They explained everything and said, ‘you’re in a good place. We have plenty of equipment and staff to take care of you.’ At the time everything on the news had been about the potential lack of ventilators and staff. So that made me feel better.”
But it was a challenging time, because the disease meant he could not have in-person visitors. Nurses set him up with family visits on his phone via Facetime, “but it wasn’t the same” as having loved ones bedside.
Even staff interactions were brief, with barriers of masks and personal protective equipment between.
“The nurses would come in several times a day and their interactions were timed, which I completely understand, to limit exposure,” he said. “But you’re in a room by yourself with no human interaction. That was a little bit difficult.”
Sometimes that even meant waiting for meals and medication to be delivered at the same time, so the care team could multitask while wearing masks and personal protective equipment.
“I know that prevented additional contact with a known COVID patient and also helped with PPE supply issues,” he said. “I understand because I am also in the medical field. But I do believe that could be an issue with those who don’t understand.”
During that trying time one night around 2 a.m., too late to call family, Fulbright took a turn for the worse and doctors consulted on admitting him to the ICU. Fulbright said he greatly appreciated a nurse “who went above and beyond.”
“Sometimes all people need is someone to sit and talk to them and be compassionate, and one UAMS nurse in particular took that extra minute to do that for me,” he said. “Sometimes it’s not medicine people need in a moment like that.”
Fulbright was treated with hydroxychloroquine, an anti-malarial drug initially approved for emergency use to treat COVID-19. However, the potential risky side effects of the drug have since led the U.S. Food and Drug Administration to withdraw its approval for emergency use.
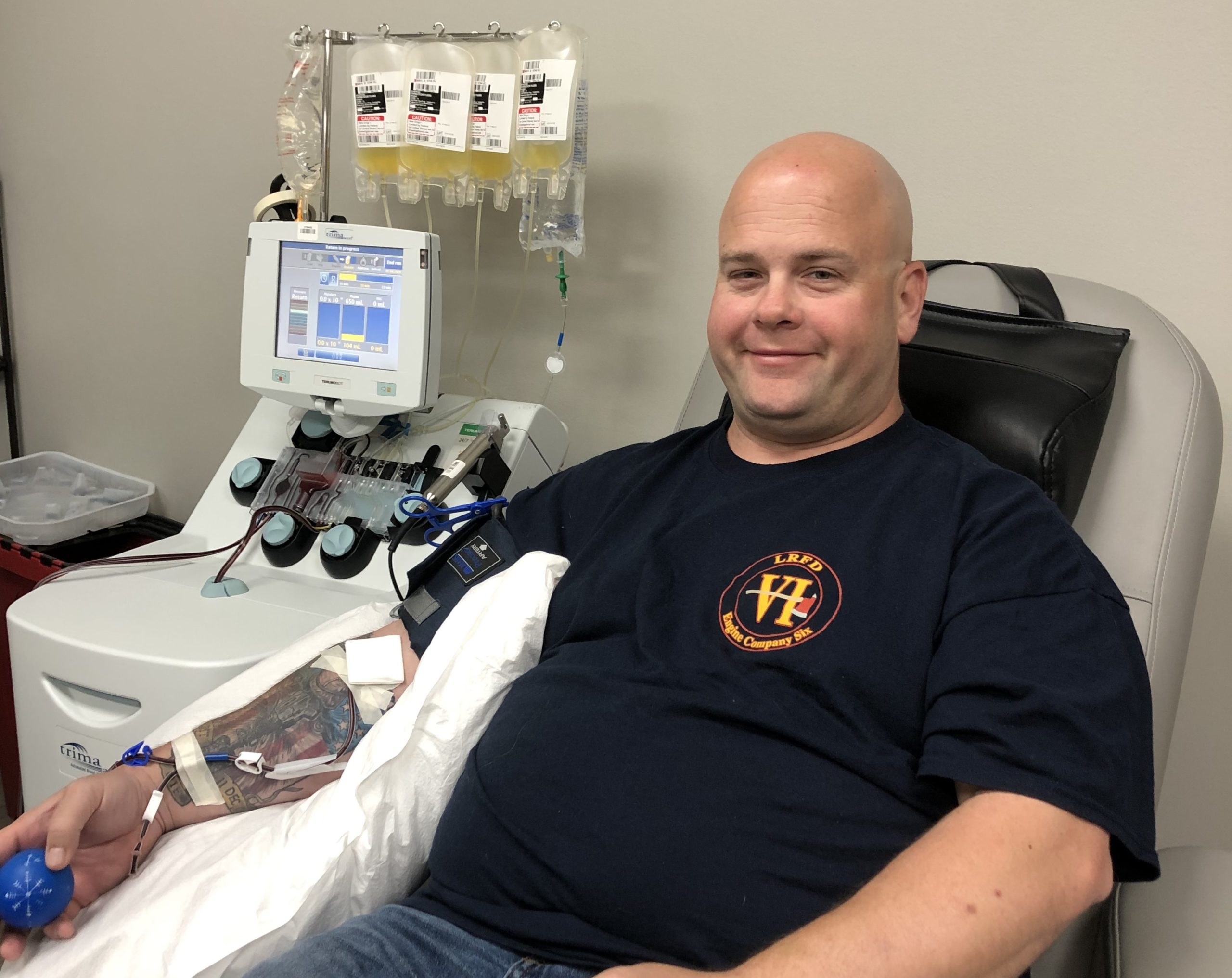
After six days, Fulbright was recovered enough to be released from the hospital into home quarantine. It would be six long weeks before he was cleared to go back to work. During that time, he signed up for a statewide program being directed out of UAMS that uses blood plasma of those who’ve overcome COVID-19 to research potential treatments to use against the disease.
“Hopefully that will help someone else who is further along in progression than I was and give them and their family another chance and some hope,” he said. “It was an hour out of my day to go and donate plasma. Hopefully that will help someone else, and they can get through COVID themselves.”
Meanwhile, he’s warning others to stay vigilant as Arkansans battle the pandemic and the state sets guidelines for reopening of schools and businesses.
“People need to be more attentive about where they’re putting their hands and washing their hands more frequently. I think that would help not only with COVID, but flu season, too. I think hand washing is the number one preventative right now,” he said. “We have to be smart while it’s out there and give ourselves time to find an answer to this problem.”