UAMS Neurosurgeon Performs State’s First Deep Brain Stimulation for Epilepsy
| The UAMS Epilepsy Center is the first in Arkansas to perform deep brain stimulation surgery as a treatment for epilepsy.
Deep brain stimulation (DBS) for epilepsy is designed to help manage seizures in patients who have not responded to medication. DBS, which is a type of neuromodulation, has been used primarily for patients with movement disorders, including Parkinson’s disease and some psychiatric disorders. The Food and Drug Administration granted approval for use of DBS therapy for epilepsy in December 2018.
The Epilepsy Center at UAMS is the only adult comprehensive level 4 epilepsy center in the state certified by the National Association of Epilepsy Centers. Sisira Yadala, M.D., is the center’s director.
“Because we are a level 4 center, our multidisciplinary team of experts are able to provide the latest and most sophisticated treatment modalities to our patients,” Yadala said. “We are proud to be able to provide patients with comprehensive care.”
Deep brain stimulation involves surgically implanting a thin wire with electrodes in specific regions of the brain. A neurostimulator device is placed under the skin below the collarbone. The device can be programed to deliver imperceptible gentle electrical pulses to the brain to help stop or reduce frequency of seizures.
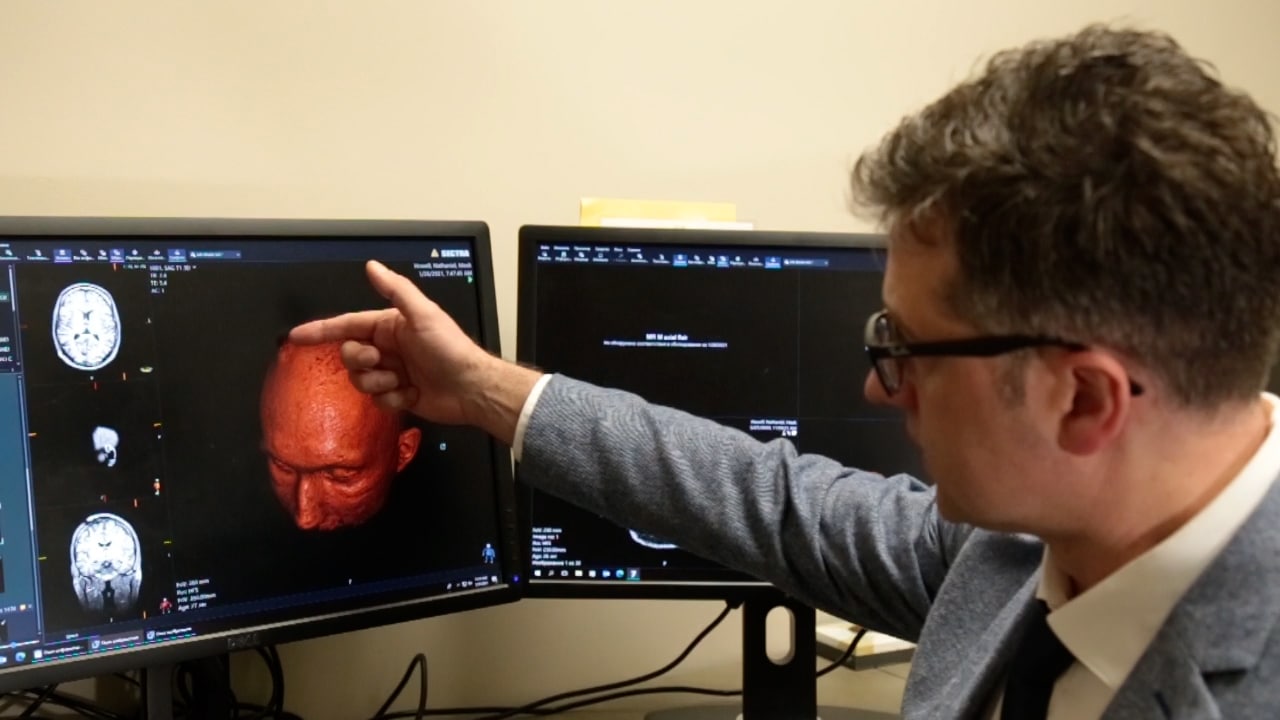
“When it comes to surgery, we have high-precision equipment including a robotic assistant and intraoperative CT scanner that help us verify the electrodes are being placed accurately,” said Viktoras Palys, M.D., a UAMS neurosurgeon and center’s surgical director.
Nathaniel Howell, 28, had his first seizure when he was 3. It was so subtle, it could have gone unnoticed. But his mother, Kecia Howell, has a sister and a niece who have epilepsy.
“The ones I remember early in life were partial seizures, but then they changed to full body ones that mostly happened at night,” Nathaniel Howell said. “We went through a litany of medicines trying to get rid of them.”
Palys says DBS surgery is the best option for patients who have not responded to medication and whose seizures come from different parts of the brain. In the past, there were few options for patients like Howell, other than vagus nerve stimulation (VNS). VNS works much like DBS, only the VNS electrode is attached to the vagus nerve in the neck and delivers gentle electrical pulses at regular intervals.
Howell has a vagus nerve stimulator, but his seizures have remained persistent. The longest he’d gone without a seizure was about two months. The Howells know firsthand how dangerous seizures can be. Brock Howell, Nathaniel’s brother, died in 2017 after he had a seizure at night. He was 25.
Nathaniel Howell was born in Mississippi. In the late 90s, his family moved to Alaska. They lived there for 13 years before moving to Piggott, Arkansas. Searching for an epilepsy specialist was top priority when they settled in. They found a pediatric neurologist, Stephen Bates, M.D., at St. Bernard’s Healthcare in Jonesboro.
“We loved him. Nathaniel saw him until he was 19 or 20,” said Kecia Howell. “Finally, Dr. Bates told us he’d have to send Nathaniel to see an adult epileptologist. He referred us to UAMS.”
That was about seven years ago. Now they see Yadala. She told them about the DBS therapy, and they were willing to try it.
“Our doctors were really good about providing us information about the procedure and the device. The results are very promising,” Kecia Howell said. “One of the hopes of for the DBS is that it will control Nathaniel’s seizures enough that we can reduce his medication and be able to turn the vagus nerve stimulator down.”
Yadala says they’re likely to see results as soon as two months after the device is turned on. And the longer the patient has the device, the better the seizure control.
“There can be improved efficacy even years down the line,” Yadala said. “Seizures happen when there is abnormal excessive electrical activity. Over time, these pulses from the DBS are able to modulate that activity and provide seizure improvement and hopefully seizure resolution. We’re happy for the potential this means for Mr. Howell and other epilepsy patients.”
Palys implanted the device in late December. Then Jan. 26, after he had healed enough from the surgeries, Howell and his mother came back to see Palys and Yadala to turn on the device and show them how it works. In addition to reducing seizures, the device will also give his physicians data to analyze when he has a seizure.
“There is a surprising number of things you cannot do in society if you have active seizures that you learn about if you live in a farming community.” Howell said. “I’m hoping this procedure will control them enough for me to at least do the things I’ve always spent time wanting to do.”