Cochlear Implant Surgery Restores Hearing, Improves Marriage
| After 26 years of marriage, Beverly Holloway still had a lot she wanted to discuss with her husband, Patrick.
But despite him taking the initiative six years earlier to obtain hearing aids, they were both frustrated that the devices were no longer working, despite repeated adjustments.
Here they were in their golden years, which are supposed to be happy, but Patrick Holloway’s increasing inability to hear cast a shadow of despair over their future. Although they longed to resume their conversations and continue sharing their adventures, they seemed to have reached an impasse.
After years of being able to freely converse about everything under the sun, Patrick Holloway’s 30 years of driving tractor-trailers, racing motorcycles with the muffler off on Saturdays and using chainsaws to chop wood had caught up with him. He was nearly deaf.
“When you’re young, you’re invincible,” he said. “You think you’ll live forever.”
“It was awful,” Beverly Holloway recalled. “We hadn’t had a conversation in years.”
Communication, however, was vital to their happiness and their marriage. So Beverly Holloway, who had worked in medical management for 30 years, began researching cochlear implants on the Internet, having heard that they helped a celebrity, Rush Limbaugh, but not knowing much else about them.
The implants are surgically implanted into the cochlea, the spiral cavity of the inner ear, and are connected to a speech processor that is worn behind the ear like a hearing aid. The processor, connected to a microphone, picks up sounds and changes them into electrical impulses that are sent to the implanted receiver, stimulating the auditory nerve.
“I kept researching, and everything — and I mean everything — came back to UAMS and Dr. Dornhoffer,” she said, referring to John Dornhoffer, M.D., chairman of the Department of Otolaryngology – Head and Neck Surgery in the College of Medicine at UAMS.
She said that at first she couldn’t believe it: this world-renowned ear, nose and throat surgeon was only 30 miles away in Little Rock. On top of that, she learned that Dornhoffer, who lectures internationally and serves on several editorial review boards, had one of the implants himself. What could be better?
Still, she said, “at that time we thought it was just for rich people.”
But, never one to give up, Beverly Holloway called UAMS to find out more, and learned that in many cases the implants are covered by Medicare.
“What a great phone call it was! Confetti should have fallen from the ceiling!” she said later, recalling the information that provided much-needed hope for the couple. She quickly made an appointment for her husband, and the next thing they knew, he was scheduled for surgery to have one of the devices implanted in his right ear.
Dornhoffer performed the surgery March 18, one day after Patrick Holloway’s 80th birthday. Then the couple returned to UAMS on April 13 to have the processor turned on. The delay allows time for swelling from the surgery to subside.
Although they were told it could take about six months for Holloway to adjust to the implant, the couple was thrilled when he began hearing, and understanding what he was hearing, that same day.
“We talked all the way home,” Beverly Holloway wrote four days later in an email to the otolaryngology team at UAMS. “That was our first conversation in three years.”
Because the implants stimulate the cochlea with electrical impulses rather than auditory ones, the brain has to learn how to interpret the new information and translate it into understandable sounds and speech. If the patient has some residual hearing, as Holloway does, the brain has to reconcile any natural hearing ability with the information provided by the implant.
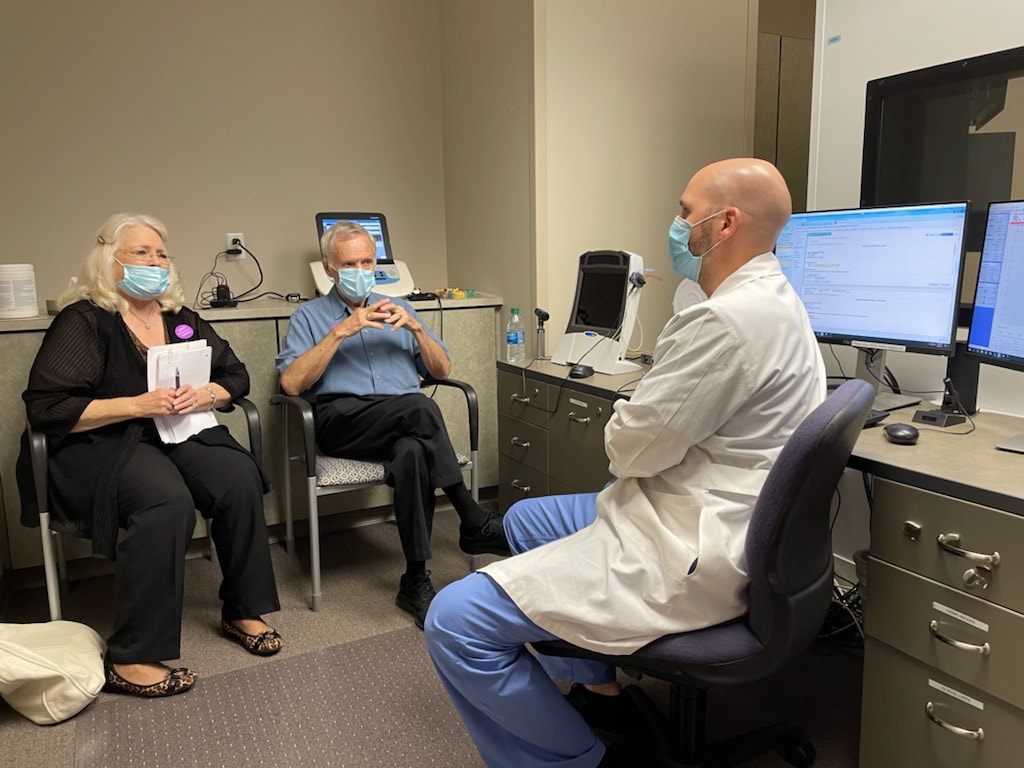
When the couple returned to UAMS three weeks later for Holloway’s follow-up appointments with speech therapist Rachel Beckham and audiologist Matthew Brown, Au.D, Beverly Holloway was still marveling about the drive home, saying, “We hadn’t had a conversation like that for years.”
At that visit, Patrick Holloway told Brown, “I can hear the clock ticking 20 feet away. I can hear birds chirping.”
But voices are more difficult, he said, explaining, “I can hear words; I just can’t hear what they are.”
Brown reassured him, “To be doing as well as you are right now is actually very good. I would not expect you to be able to hear everything right now.”
On hearing tests at that appointment, Holloway scored 78%, Brown said, a “a huge difference” when compared with the 16% he scored before the surgery.
Brown also told Patrick to wear just the implant, without a hearing aid in his other ear, to allow for adequate rehabilitation of the implant. In subsequent visits, Brown will assess performance with the cochlear implant. Once a stable program is achieved, the audiologist will introduce a hearing aid for the opposite ear. Then performance can be further measured with the use of both cochlear implant with hearing aid versus cochlear implant only.
Dornhoffer said that while Patrick Holloway’s adjustment to the implant has been “better than some,” it typically takes about three months for patients to really understand what they’re hearing, and six months to fully adjust.
“It’s like learning a new language,” he said. “You have to kind-of sort out in your brain what these new sounds are.”
“He’s doing well,” Dornhoffer said about Holloway.
Dornhoffer said some adults end up getting implants in both ears, but most prefer just one, while continuing to use a hearing aid in the other ear, especially if they have come to rely on their residual hearing and the hearing aid for listening to music or certain low tones. Cochlear implants don’t translate sound into as many tones as the human ear does, which can make it difficult to listen to music.
On the other hand, he said, about 90% of children with serious hearing loss will get cochlear implants in both ears.
Dornhoffer received his cochlear implant in 2015 and said he has been debating whether to get a second implant. He has some residual hearing and isn’t eager to have that destroyed, which has to be done to implant the cochlear device.
As one of only four implant surgeons in the country who has an implant, Dornhoffer said he has a unique sense of empathy with his patients. For him, he said, “it’s more than just a job. It provides a different motivation.”
Dornhoffer also is a member of the board of directors of the American Cochlear Implant Alliance, whose mission is to use research, advocacy and awareness to advance access to hearing through cochlear implantation.
“There’s a real issue in Arkansas, where less than 10% of people who would benefit from cochlear implants actually get the implants,” he said. “One of our missions is to understand why.”
Cost is a big factor, he said, but many people don’t realize that Medicare covers 80% of cochlear implantation while supplementary Medicare covers the rest.
“It doesn’t cover hearing aids, but it does cover cochlear implantation,” he said.
For the Holloways, the surgery couldn’t have come at a better time.
“It’s been a 150% wonderful experience,” Beverly Holloway said. “I have never been to a hospital that’s so courteous and so patient-friendly. That place really does care about people, and they truly make it an easy experience.”
As she wrote to the UAMS team, “You cannot know how happy you make your patients. You are giving new life, new happiness, new chances to people who would have otherwise been in pure despair.”