View Larger Image
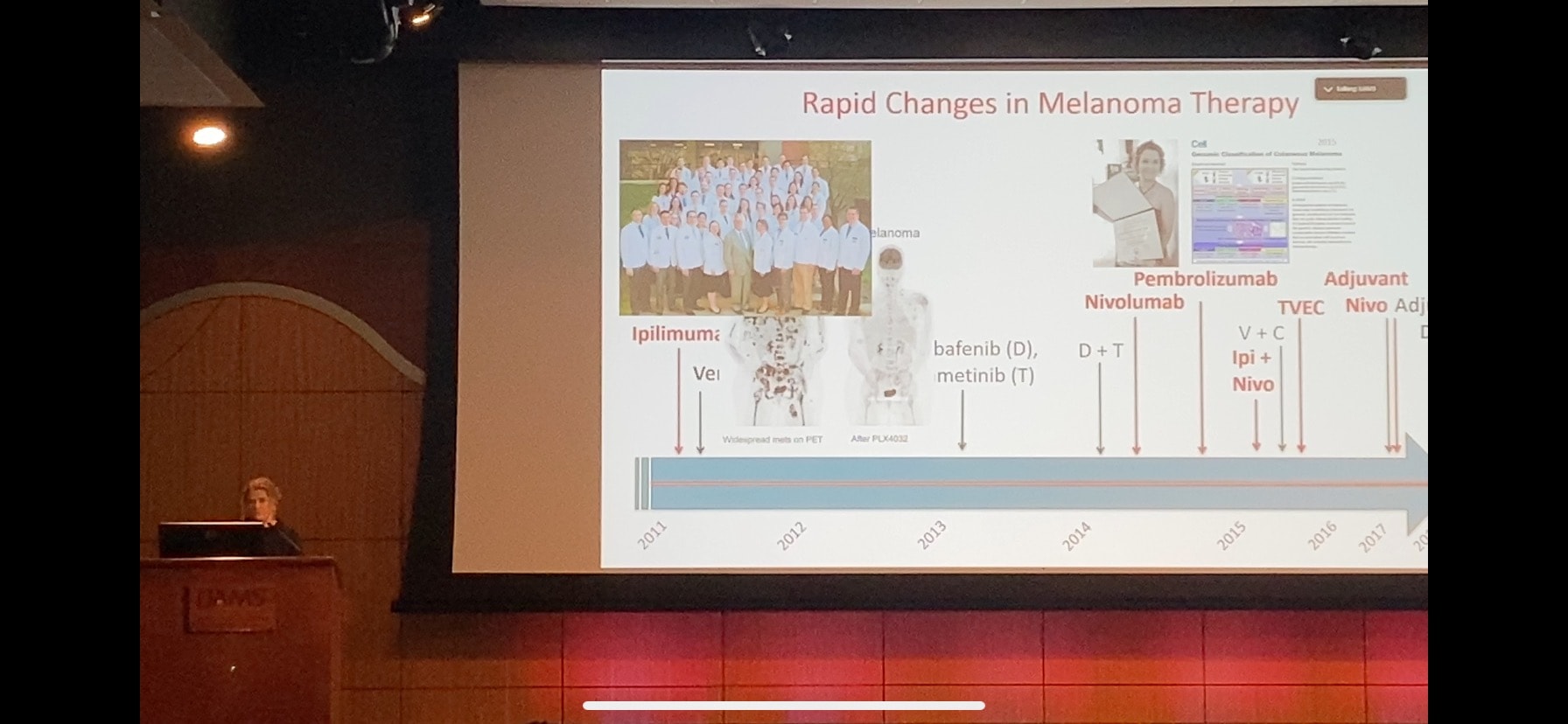
Genevieve Boland, M.D., Ph.D., discusses advances in melanoma treatment.
Harvard Researcher Discusses Melanoma Treatment Options during Annual Lecture
| May 18, 2023 | A cancer surgeon and researcher from the Massachusetts General Hospital and Harvard Medical School, whose work focuses on maximizing the surgical and medical treatment options for patients with melanoma, was the guest speaker May 5 at a lunchtime lecture at the University of Arkansas for Medical Sciences (UAMS).
The talk by Genevieve Boland, M.D., Ph.D., in the UAMS Jackson T. Stephens Spine & Neurosciences Institute’s Fred Smith Auditorium was part of the Colonel William “Randy” Holland Memorial lecture series on melanoma, the deadliest form of skin cancer.
It was timed to coincide with the beginning of May, which is Skin Cancer Awareness Month.
The series was established in 2008 by friends and family members of Holland, a lifelong Arkansan who retired in 2005 after 42 years with the Arkansas Army National Guard, where he was a helicopter pilot. Holland died in September 2007 from Stage IV malignant melanoma.
Boland, a physician-scientist surgeon who specializes in melanoma and cutaneous oncology, discussed an ongoing “explosion” of advances in treating the deadly form of cancer, which the American Cancer Society estimated will result in nearly 100,000 new diagnoses nationwide in 2023.

Boland and Shalin flanked by Thomas Jennings, M.D., an assistant professor of dermatology at UAMS, and Matthew Steliga, M.D., a professor of surgery at UAMS.
“The goal of this lectureship is to increase awareness of melanoma prevention, diagnosis, treatment and research,” Sara Shalin, M.D., Ph.D., who chairs the UAMS College of Medicine Department of Dermatology, said in introducing Boland.
“I am grateful for the presence in our audience today of Mrs. Leslie Holland, Col. Holland’s wife; her sister, Robin; as well as dear friends Dr. Bob Burns and Mary Lindsey, both of whom had long careers at UAMS before their own retirement,” Shalin said.
Boland, an associate professor of surgery at Harvard Medical School and section head of melanoma/sarcoma surgery and vice chair of research at Massachusetts General Hospital, has been instrumental in helping to understand how and why some patients respond or don’t respond to certain therapies as well as what can be done to identify patients most at risk for developing advanced disease.
She discussed early advances in cancer therapy and immunotherapy, saying that it wasn’t until about 2014, when she was working at the M.D. Anderson Cancer Center in Houston, Texas, that “things started to perk up” in terms of research and clinical trials.
Boland emphasized the importance of a multidisciplinary approach, like that used at UAMS, to provide coordinated options for melanoma patients.
“For the first time, the overall number of deaths from melanoma is going down,” Boland said. “We need to think about how to make this more equitable, how to make sure more patients have access” to drugs that activate the immune system to defeat cancer.
Boland called on physicians and researchers to be persistent in the quest to find treatments.
She said Steven Rosenberg, M.D., was thought to be crazy when, in 1968, he transfused one patient’s blood into another patient, in an effort to prompt the second patient’s immune system to behave like the first patient’s immune system and destroy his cancer. The effort failed, but Rosenberg forged ahead, and many years later he was recognized for pioneering the development of effective immunotherapies and gene therapies for patients with advanced cancers.
“As a surgeon, I’m proud of the persistence in the surgical community,” Boland said.
“In 2011, the FDA approved the first immunotherapy and targeted therapy drugs for melanoma,” Shalin said. “This has changed the landscape of dermatology and cutaneous oncology, and for the first time, in the last few years we are seeing patients with metastatic melanoma achieve partial and complete remissions from their disease. Those of us working in this space are excited about the pace of discovery and continued acceleration of treatment options and the resultant improvements in survival of our patients.”