View Larger Image

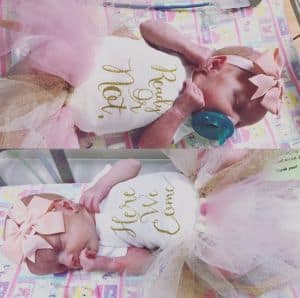
Charlotte and Emelia Dubs with their parents Kenzie and Morgan.
Multi-Disciplinary Structure Provides Best Care for Maternal Fetal Medicine
| Charlotte and Emelia Dubs are just starting to toddle around their world. The 1-year-old twin girls from Conway spend their days exploring, laughing, blowing kisses and keeping their parents, Kenzie Butcher-Dubs and Morgan Dubs, on their toes.
The Dubses have seen many milestones over the past months. And as the family prepared to celebrate the babies’ first birthday earlier this year, Butcher-Dubs thinks back on the hours leading up to their birth and the possibly tragic outcome had it not been for access to specialists at UAMS.
She didn’t feel quite like herself on the day before she was to be induced. She’d been on modified activity since week 23. On the day of her last checkup, everything appeared to be fine.
“I later started feeling pretty rundown, but I was very pregnant and had been running around doing last minute chores. So I figured that was to be expected,” she said. “But that night I started experiencing some weird symptoms.”
She was more nauseous than normal, experienced heartburn (which had not been typical for her) and increased swelling in her legs. She’d drank a lot of water that morning, but hadn’t produced much urine.
“If I hadn’t been scheduled to go in the next morning to be induced, I would have gone in that night,” Butcher-Dubs said. “I knew the signs of pre-eclampsia and I knew that I had some of them but my blood pressure was fine, and that’s a main indicator. I figured there was really nothing to worry about.”
Pre-eclampsia is a condition in pregnancy where there is a sudden rise in blood pressure. It’s can lead to serious or fatal complications. The following morning, Butcher-Dubs says she felt worse. Within a few hours of arriving at UAMS, her blood pressure became in the severe range.
Her lab work showed her kidneys were beginning to fail. She was diagnosed with pre-eclampsia.
“Pre-eclampsia can happen in about 10 percent of pregnancies,” said Pamela Simmons, M.D., a maternal-fetal medicine fellow in the UAMS College of Medicine Department of Obstetrics and Gynecology. “It generally happens in the third trimester; however, it can happen any time during the pregnancy generally after 20 weeks.”
Butcher-Dubs was also diagnosed with a hemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome. HELLP is a serious complication of high blood pressure that sometimes accompanies pre-eclampsia.
Her labor and delivery was accompanied by nausea and vomiting. “After I delivered Charlotte, I actually lost consciousness because of how sick I was. Things became very critical and Emelia had to be delivered via vacuum. She was born not breathing and had to be resuscitated.”
Kenzie-Dubs spent several days in the hospital following the delivery. The babies, born at 36 weeks, spent 14 days in the neonatal intensive care unit.
“The great thing about UAMS is that all the specialists and subspecialists are under one roof,” Simmons said. “A lot of things went right for Kenzie and there are many stories like hers. We all work together well and are able to efficiently access a patient’s needs.”
The group includes experts in neonatology, urology, cardiology, anesthesiology and nursing, as well as therapists and lactation consultants.
Simmons says at UAMS multiples are delivered in an operating room as a precautionary measure. Butcher-Dubs did not have a cesarean section, but all the resources and people were there in case it became necessary.
“Mrs. Dubs had various different risk factors that could have led to a C-section,” Simmons said. “Her pregnancy was unique in that the twins shared one placenta. But they were both head down and labor was quick. That was favorable. We like to have a natural delivery, but we like to have the proximity of the operating room for safe-keeping.”
If given the chance to do it again, Butcher-Dubs says she would have come to the hospital as soon as she started having symptoms. She urges expecting mothers to listen to their bodies.
“I didn’t want to be that overly worried pregnant lady who shows up at the hospital for every little thing,” she said. “But it would have been absolutely worth feeling stupid had it just been a false alarm. We were incredibly blessed to come through our experience with all three of us eventually healthy. But my decision to brush off my worries could have easily ended in a different outcome. If you think something might be wrong, go get checked out. It could be the difference between a very happy ending or a very scary one.”