Nursing In COVID-19: What It’s Like at UAMS
| The World Health Organization declared 2020 as “The Year of the Nurse and Midwife” in honor of the 200th anniversary of Florence Nightingale’s birth on May 12, 1820. UAMS is honoring “200 Years of Nursing and 365 Days of Caring” by sharing six UAMS nurses’ responses to a series of questions about working on the front lines of COVID-19.
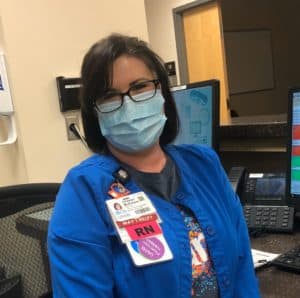
These nurses are Jeff Crowson, an infection prevention specialist; Andrew Estrada, Advanced Practice Partner in the Oncology/Transplant Division; Julie Kemp from the Maternal Fetal Medicine pod in the UAMS Women’s Clinic; Carrie Knauer from the Emergency Department; Sarah Launius from the Intensive Care Unit on E4; and Christel McEntyre from One Day Surgery Preop, who was redeployed to the recovery room Intensive Care Unit and also served as a nurse liaison to help patients and their families communicate.
What are the biggest changes in your job since the COVID outbreak?

Julie Kemp
JULIE: We are paying close attention to making sure our environments are clean for both staff and our patients along with making sure we are following the most up-to-date recommendations from leadership. Our pregnant moms are not able to have their guests with them during their appointments, so as nurses, we get to step in and do our best to fill some of that void.
CARRIE: Everything has been a big change! The visitor policy, the employee screening policies, the ever-changing policies regarding PPE … approaching every patient as they could possibly be infected – including trauma patients. How we communicate with patients’ family members has changed since they are not able to be at bedside. It is all very mentally and emotionally draining.
SARAH: There are so many changes we’ve experienced since COVID-19 started. First, we have had to completely change the way we provide family-centered care. As we all know, family is unable to be at the bedside during this time. With any patient, this is difficult for them, but especially those requiring ICU care. Often, the patients are unable to consent for themselves, and not having a family member there to represent them is tough. Most of our interaction with family now is done via Facetime or phone calls. I’m thankful we have the technology available to do this, but it is very different.
Another big change that has affected our job is making sure we are always up-to-date on the current Personal Protective Equipment guidelines. This is so important for us, so we know that we are safe to take care of our patients, and so we are safe going home to our families. When we come to work and get assignments, we must prepare our PPE for the day before doing anything else. This has changed our work flow a bit, but we have learned to adapt and continue to provide the best possible care to each and every patient we encounter.
What do you miss the most?

Jeff Crowson
JEFF: Knowing the answers to most questions.
CARRIE: Everything seemed much easier before COVID. I do miss not having to wear a mask every single day!
ANDREW: I miss the in-person meetings with my colleagues. I think we are fortunate to live in a digital age where accessibility to each other is a few keystrokes away; however, I believe the personal touch of face-to-face meetings are lost.
JULIE: I miss our moms being able to celebrate with their partners when seeing their baby on ultrasound for the first time.
What are the biggest lessons learned?
CHRISTEL: Now more than ever, nurses have to be both a nurse and emotional support for patients and families because of the no visitor policy.
JEFF: You can never be too prepared. There are many aspects of care and many products that we have taken for granted. Are we consistently caring for patients in the safest manner? Are we thinking of everything? Will we always have products available, even when everyone needs greater quantities of the same supplies? Suddenly, we have had to think creatively every day.
CARRIE: The importance of keeping yourself protected!

Sarah Launius
SARAH: One of the biggest lessons I think we’ve all learned is how being prepared is so important. I know that as a hospital we have prepared tremendously after this virus was found in the state. They’ve created a whole new unit to care for those ill with this virus. I think we’ve all learned a lesson in preparedness as a nation. With the worldwide shortage of supplies, I’m thankful that so far we’ve had what we need to provide safe care. I bet that when this is over, we will be preparing in the event we see something like this again.
Another huge lesson I’ve learned personally is how important families are to provide the best care to patients. In the past, the family has always had the ability to be present in the ICU. With new restrictions, we are being creative with Facetime and frequent phone calls to be able to connect patients and their loved ones. We are being support for patients in a different way, “standing in” for their family when they cannot be by their side.
Who or what have you learned to appreciate?
CHRISTEL: UAMS

Carrie Knauer
CARRIE: I have learned to appreciate my co-workers even more! We have always been close. We deal with so much illness and trauma together, but this has brought us even closer. We have really “been through” something together now … we are handling this, and we are doing it together.
JEFF: Supply Chain and the amount of work it takes to keep the hospital running. The willingness of everyone at UAMS to bring their best game and do whatever it takes to get through this.
SARAH: Our leadership! Our ICU leadership, Ed Horton and Elizabeth Sullivan have been amazing throughout this. They’ve put in more hours and spent time with each of us helping us to learn and make sure that we feel safe caring for the patients on our unit. Elizabeth has even stepped in to allow me to take a lunch break on a day when we were short staffed and super busy. People are going above and beyond their job “title” to help us, and I am so appreciative of that.
What do you wish you had more of?
ANDREW: I wish I had a knack for sewing so I could make face masks. I find the dedication of my work colleagues and members of the local community inspiring when they provide their time and efforts to serving others through their talents.
CHRISTEL: I hope after we are redeployed back to our unit to work with elective cases, the department finds a way to continue the role of the nurse liaison. We have seen a positive response, and it focuses on patient-centered family care.
Please share a patient experience during this time that stands out in your memory.
JEFF: Our first patient to test positive for COVID-19. That’s when we knew the situation was real.
ANDREW: I had a recent encounter with a patient I cared for when they were initially diagnosed with multiple myeloma. We had grown very close during the early stages of their treatment. I remember reassuring them that they were at one of the best institutions for their treatment and that they were a part of our UAMS family now. I think in some small way it helped them overcome their initial rounds of treatment with newfound confidence. I had been feeling unsure of myself after taking on my new position, but despite the fear and vulnerability they might be feeling during these trying times, this patient returned that same reassurance to me when I encountered them on the inpatient unit a few weeks ago. It was a touching moment for me, and I think it’s easy to forget how patients have their own way of providing care for their nurses.
Christel McEntyre
CHRISTEL: A young lady who came in as an emergency case hadn’t been in contact with her family and had no cell phone. When we got the telephone number to her parents, we were able to use Facetime and give them reassurance that their daughter was being taken care of. The parents had not been able to locate their daughter within the UAMS system. We were able to provide a means of communication between them and gave them updates during her surgery, recovery and when she went back to the inpatient unit.
SARAH: This time has been especially hard when we lose a patient. One memory that stands out to me is when we had a patient whose family made the difficult decision to transition to end-of-life care. This is something we do often on our unit, but in the present time it is made much more difficult by the fact that the family is often unable to be by their loved ones side. In this particular circumstance, the family asked us to play a favorite song the patient could hear as they passed. I was not the nurse for this patient, but one of my amazing colleagues was able to play the song over the patient’s room speaker, and another nurse stayed in the room with them until the patient passed so they wouldn’t be alone.
What are you looking forward to when this is over – at work?

Andrew Estrada
ANDREW: I cannot wait to see everyone’s smiling faces again. While I appreciate the safety and creativity of using face masks, I miss those personable exchanges we all had. It has only been a few weeks but it’s astounding how such a simple barrier can affect one’s ability to fully connect with others. I’m trying to learn to smile with my eyes, but it is a difficult technique to master.
JULIE: I’m looking forward to not wearing masks and being able to see our patients smile!
SARAH: Honestly, I’m looking forward to not wearing a mask for 12.5 hours out of the day. I’m thankful that we have rules to keep us safe, but it will be nice to breathe the fresh air once again.
What are you looking forward to when this is over – at home?
ANDREW: I am looking forward to the spontaneity of being able to plan outings with friends and family again. I feel it is important to be judicious with gatherings, to not only protect our loved ones but also our community.
SARAH: I’m looking forward to going back to my pre-COVID routine. When this started, I packed a “go-bag” in my car. This is in the case we have a surge of COVID-19 patients, and I feel that I need to stay away from home to protect my family. So far, we’ve had enough negative pressure rooms on our unit that I feel safe going home with a strategic decontamination plan. When I get home from work now, I leave my shoes, badge, keys, and wedding band in a box in my garage. I sanitize each item before putting it in the box. I sanitize my steering wheel, my seat, literally anything I touched on the ride home. I Lysol the car, too. Then, I undress before even entering my home. My husband opens all the doors for me from the garage to the shower, and turns it on so I don’t touch and contaminate things in my home. I have even been using our spare shower, so that my husband and son don’t shower where I do. I have a one-year-old, and one of my biggest fears has been bringing anything home to my family. So, when this is over, I will be so thankful to get to go back to being able to touch a doorknob in my own home without fear.
CHRISTEL: Visiting and hugging my family members and friends.
JEFF: Sleep and a little time off.
CARRIE: I have enjoyed my time at home with my family and will continue to do so.
How do you think this experience will change the role of nurses going forward?
SARAH: I think this experience has really put the role of the nurse in the spotlight. None of us go into nursing for the accolades; we do this because we have a heart for helping others. The public oftentimes has no idea what the role of the nurse is. This pandemic has shed some light on what our job is publicly, and I do feel that people have become appreciative of what we do overall.
ANDREW: I am hoping this experience serves as a moment of reflection and empowerment for nurses. I hope that nurses realize how integral they are to the nation’s health care system, and they are shining lights of inspiration in these dark times. We are stronger united, and I hope we all grow from this and continue to make positive changes to our communities in the future.
CHRISTEL: We’ve had to become more aware of our usage of PPE as well as monitoring more handwashing and donning and doffing procedures to help keep our patients and co-workers safe. We have had to monitor whether or not patients have been properly screened prior to entering the hospital and whether or not they have had a positive test.
JULIE: I think nurses will always be viewed as a highly valuable and vital resource in health care. I think it has established our confidence in our role both within the profession and in the public’s view of the profession.
CARRIE: If we can make through the first pandemic, we can make it through anything. Nurses are the best at adapting and overcoming!
What in your nursing training/experience prepared you for this?
CHRISTEL: This is unprecedented in our lifetime. Nothing really has really prepared me for this pandemic; however, I have learned a lot, and I am becoming a stronger nurse.
JULIE: Our manager and hospital in general has trained us to remain calm in the face of scary situations, to take control and apply our nursing knowledge and to always put safe and quality patient care at the forefront of what we do every day.
ANDREW: I feel that washing my hands and the correct application/removal of PPE has been reinforced since I began my nursing career at UAMS. Our oncology population are some of our most vulnerable patients and being diligent in protecting them is a lesson I always carry with me. I find it comforting to know how knowledgeable our health care personnel are in infection prevention and how they are instrumental in flattening the curve to protect our community.
How have you and your co-workers adjusted to all the changes?
ANDREW: I have never been more proud of my co-workers and their adaptability in these trying times. The level of patience they have shown as new changes are thrust upon on them on a near daily basis is such an inspiration to me. I am so fortunate to be a part of a wonderful team that inspires me daily.
JEFF: We have worked more and harder than we ever imagined we would. It’s been a constant synthesizing of information and situations in order to make the safest environment we can for our health care workers and patients.
CARRIE: There has been confusion, emotions, frustrations and some tears have been shed, but we are keeping our heads up, working as a team and doing the best we can.
Anything else you’d like to add?
CHRISTEL: I have never been more proud to work at UAMS.
JULIE: We are truly blessed to work at UAMS!
SARAH: These times are different and new to each of us, but I’m thankful that when I go to work, I have the support of my peers and our leadership at UAMS. There’s no one else I’d rather face a pandemic with than the people I work with on E4! I’d also like to add how appreciative I am of our community! From prayer, to donations of meals, masks, scrub caps and ear savers, the community has stepped up in a huge way. I think I can speak for every one of us in saying a huge thank you to those who have supported us in this fight!
