View Larger Image
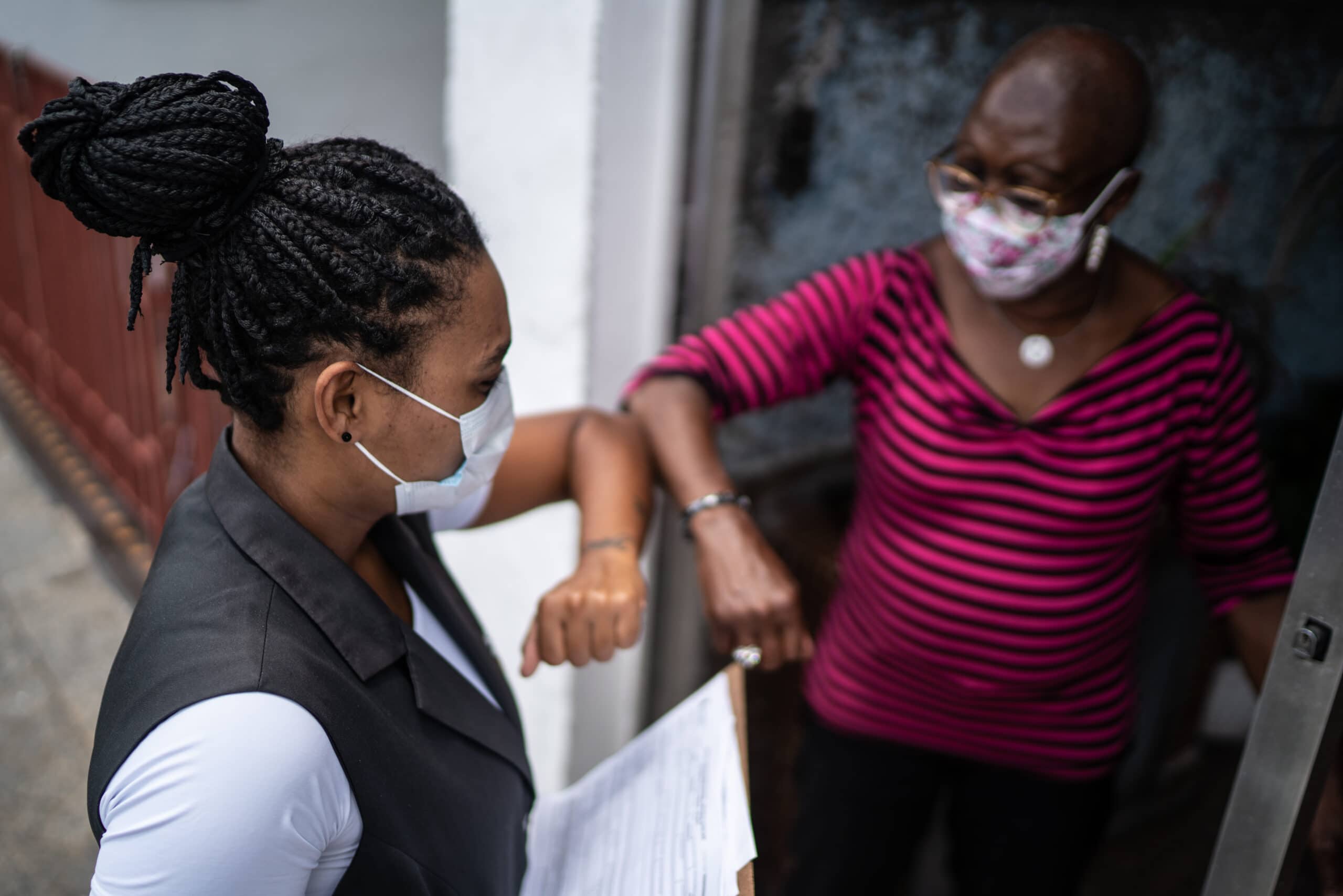
Heart Healthy Communities workers gather information from community members.
UAMS Heart Healthy Communities Project Teams Up with UCLA, Howard University Researchers
| LITTLE ROCK — The University of Arkansas for Medical Sciences (UAMS) Heart Healthy Communities Project is partnering with researchers at the University of California-Los Angeles (UCLA) and Howard University to proactively engage historically marginalized and disadvantaged populations, and provide crucial information and resources during public health crises.
The goal is to improve the quality and length of lives in the community.
Poor health outcomes disproportionately impact underserved, low-income communities. The UAMS Heart Healthy Communities’ mission is to improve health outcomes among impoverished rural populations by deploying community health workers to engage residents and determine which health and social services are needed to improve health outcomes, said Irion “Chip” Pursell Jr., MPH, RN, principal investigator for the project.
Assisted by a $1.7 million grant from the CDC Foundation, the UCLA and Howard University researchers launched Project REFOCUS (Racial Ethnic Framing of Community-Informed and Unifying Surveillance) in October 2020 to study COVID-19-related stigma and discrimination in underserved communities and provide related real-time information through an electronic dashboard. The dashboard is intended to be easily accessible to public health officials, the public and policymakers to help them build trust with — and respond to — the communities.
Through its ongoing work with local community health workers, the UAMS Heart Health Communities project will add actionable health and social data to the dashboard, said Pursell.
“The goal would be to determine which types of information to include, guided by input from the community, to assess the feasibility of integrating the data, and to see if/how local officials might use the dashboard with the additional data to inform their efforts to improve health locally,” said Chandra L. Ford, Ph.D., who leads the UCLA researchers.
Even before Heart Healthy Communities became one of only six projects in the country selected to work with Project Refocus, it developed a network of local providers and other community partners to connect people in the designated Arkansas communities with resources to improve health and wellness.
“Poor health outcomes tend to cluster in low-wealth neighborhoods, and the HHC community-centric approach facilitates the collection of actionable data that can be integrated into the Project Refocus dashboard,” said Pursell. “This will inform local stakeholders’ efforts to improve community health and well-being, and monitor the impact of COVID-19 and future public health emergencies.”
“Public health practitioners face challenges in effectively monitoring the presence, spread and impacts of COVID-19 among these disadvantaged populations,” said Ford, who is the founding director of the UCLA Fielding School of Public Health’s Center for the Study of Racism, Social Justice & Health, and a professor in the UCLA Department of Community Health Sciences.
“Lessons learned from prior epidemics, such as HIV/AIDS, make it clear that stigma and mistrust slow disease mitigation efforts among the most disadvantaged populations, contribute to mistrust of public health messages, delay access to services and reduce adherence to treatment,” she added. “This mistrust is rooted not in science denialism, but in legitimate concerns about the unequal treatment African American and other communities have received in health care.”
Monica Ponder, Ph.D., an epidemiologist and assistant professor of health communication at Howard University, noted that “during crises, fear can have a counter effect on access and adherence to community-level mitigation efforts.”
“Chronic stress is an important pathway by which stigma influences physical and mental health,” she said. “That can become a vicious cycle, fueled by racism and bias. Public health crisis communications must recognize the historical trauma, lived experiences and political climate in which people reside.”
The CDC Foundation is an independent, nonprofit organization created by Congress to mobilize philanthropic and private-sector resources to support the work of the Centers for Disease Control and Prevention and the public health community.
This project is supported by the Centers for Disease Control and Prevention of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $6,827,718.00 with 100 percent funded by CDC/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS, or the U.S. Government.
UAMS is the state’s only health sciences university, with colleges of Medicine, Nursing, Pharmacy, Health Professions and Public Health; a graduate school; a hospital; a main campus in Little Rock; a Northwest Arkansas regional campus in Fayetteville; a statewide network of regional campuses; and eight institutes: the Winthrop P. Rockefeller Cancer Institute, Jackson T. Stephens Spine & Neurosciences Institute, Harvey & Bernice Jones Eye Institute, Psychiatric Research Institute, Donald W. Reynolds Institute on Aging, Translational Research Institute, Institute for Digital Health & Innovation and the Institute for Community Health Innovation. UAMS includes UAMS Health, a statewide health system that encompasses all of UAMS’ clinical enterprise. UAMS is the only adult Level 1 trauma center in the state. UAMS has 3,485 students, 915 medical residents and fellows, and seven dental residents. It is the state’s largest public employer with more than 11,000 employees, including 1,200 physicians who provide care to patients at UAMS, its regional campuses, Arkansas Children’s, the VA Medical Center and Baptist Health. Visit www.uams.edu or uamshealth.com. Find us on Facebook, X (formerly Twitter), YouTube or Instagram.
###
