Greenwood Officer Rediscovers Sound with Cochlear Implant
| Greenwood police officer John Michael O’Mara has been dealing with hearing loss since childhood. For years, he tried all manner of traditional hearing aids, but he just didn’t like the way they performed.
“I was stubborn and refused to wear hearing aids,” O’Mara said. “I didn’t like the way that it sounded like a 1960s television in the background all the time. They just didn’t really fit my particular type of hearing loss.”
His hearing loss worsened over time, but it didn’t stop O’Mara from continuing in his family’s footsteps of public service.
“My family actually has about 12 people who have been in law enforcement through several generations, working for a total of 19 departments,” O’Mara said. “I think I’m sixth or seventh generation.”
Despite being fully capable of carrying out the duties of a police officer, O’Mara said some tasks were not the easiest for him. Interviews, for example, could be challenging.
“I absolutely hated interviewing people because I knew that they would be saying things, and I’d have to ask them to repeat themselves several times,” O’Mara said.
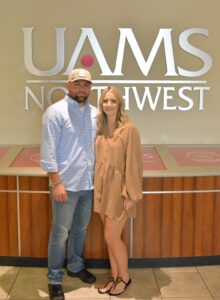
That’s not the case anymore. In June 2023, O’Mara received a cochlear implant from the University of Arkansas for Medical Sciences (UAMS). John L. Dornhoffer, M.D., an otology and neurotology physician and chair of the Department of Otolaryngology — Head and Neck Surgery, performed the procedure.
Dornhoffer’s primary focus is treating disorders of the middle and inner ear, and he has developed numerous innovations to address hearing loss, whether that loss is due to a perforation of the ear drum (his innovative cartilage tympanoplasty technique), destruction of the hammer-anvil-stirrup hearing bone mechanism (the Dornhoffer Total Ossicular Replacement Prosthesis, Partial Ossicular Replacement Prosthesis, and Footplate Shoe), or the result of chronic disease of the middle ear (his modified mastoidectomy technique).
Dornhoffer has performed hundreds of corrective procedures for patients with audiological deficits, including cochlear implantation and BAHA (bone-anchored hearing aid) placement.
Dornhoffer is very familiar with O’Mara’s situation, having experienced the same type of hearing loss and getting a cochlear implant himself.
O’Mara’s UAMS audiologist, Caitlyn Crowder Jenkins, Au.D., said hearing aids were no longer providing the audio capabilities that O’Mara needed. A cochlear implant, however, sends audio signals to parts of an ear that acoustic hearing aids cannot.
“Traditional hearing aids are really helpful for people until they reach a certain severity level of their hearing loss,” Crowder Jenkins said. “Once they reach that point, no amount of traditional amplification can give them the information that they need.”
According to Crowder Jenkins, a cochlear implant has two parts to it. One part, an electrode, is surgically implanted into the cochlea. The other part is a processor that the patient wears on the outside of their head. The processor also has two parts, one that goes on the patient’s ear and a magnet that sits a little farther up on the head. The magnet connects to the internal part and sends signals to the electrode.
“So it kind of bypasses the traditional outer ear, middle ear, inner ear, and goes straight to the auditory nerve,” Crowder Jenkins said. “It’s a different way of hearing, but it’s been really successful.”
The implant procedure is a 1 ½ hour outpatient visit. The surgeon makes a 1 ½ inch incision behind the ear, folds it forward, and then drills through the bone behind the patient’s ear to place the electrode. The patient goes home that same day with a wound covering.
“It’s pretty painless and simple,” Crowder Jenkins said. “The patient comes back about two weeks after surgery, and that’s when we turn on all of the equipment for the first time.”
One month after the implant was activated, O’Mara’s ability to understand speech went from 10% to 90%.
O’Mara said that following the procedure he is now a better communicator as a police officer and can hear things he hadn’t been able to before, like the beeping of a car when warning the driver to put on a seatbelt.
“They said that I made phenomenal progress and that I was way ahead of the curve of where I was supposed to be,” O’Mara said. “They actually canceled my six-month appointment, and I haven’t been back since, but it has been a huge change.”
The Audiology Clinic at UAMS is unique compared to other centers in Arkansas, Crowder Jenkins said.
“We take a core rehabilitation approach to hearing loss,” she said. “And we work closely as a team with both our ear, nose and throat surgeons, as well as our speech/language pathologists to get the patients up and running and understanding as quickly as possible and back in the workforce, or homelife, or school or whatever it is they do.”
“Results are different for each patient,” she continued. “Research shows that patients who have fewer health problems, like heart issues, ear problems, autoimmune diseases or cognitive issues, tend to hear and understand around the first month after activation.”
Crowder Jenkins emphasized that unaddressed hearing loss can lead to a poorer quality of life with challenges in physical and mental health, personal relationships, career growth and earning potential, and cognitive abilities with aging.
“The first step is just getting treatment, whether that is getting a cochlear implant or not,” she said. “We really look at speech scores to determine if someone is a good candidate for a cochlear implant. “If they are wearing their hearing aids and scoring 60% or less with their hearing aids on, that’s when we think, okay it’s time to start looking at a cochlear implant.”